Rubin HA, Bruce S, Rosen T, McBride ME. Evidence for percutaneous inoculation as the mode of transmission for chromoblastomycosis. J Am Acad Dermatol. 1991 Nov. 25(5 Pt 2):951-4. [QxMD MEDLINE Link].
Ahmed SA, Bonifaz A, González GM, Moreno LF, Menezes da Silva N, Vicente VA, et al. Chromoblastomycosis Caused by Phialophora-Proven Cases from Mexico. J Fungi (Basel). 2021 Jan 29. 7 (2):[QxMD MEDLINE Link].
Castro LG, Pimentel ER, Lacaz CS. Treatment of chromomycosis by cryosurgery with liquid nitrogen: 15 years' experience. Int J Dermatol. 2003 May. 42(5):408-12. [QxMD MEDLINE Link].
McGinnis MR. Chromoblastomycosis and phaeohyphomycosis: new concepts, diagnosis, and mycology. J Am Acad Dermatol. 1983 Jan. 8(1):1-16. [QxMD MEDLINE Link].
Medlar EM. A cutaneous infection caused by a new fungus Phialophora verrucosa with a study of the fungus. J Med Res. 1915. 32:507-22.
Odds FC, Arai T, Disalvo AF, et al. Nomenclature of fungal diseases: a report and recommendations from a Sub-Committee of the International Society for Human and Animal Mycology (ISHAM). J Med Vet Mycol. 1992. 30(1):1-10. [QxMD MEDLINE Link].
Terra F, Torres M, Fonseca Filho O. Novo tipo de dermatite verrucosa; micose por Acrotheca com associado de leishmaniose. Brasil Medico. 1922. 36:363-8.
Lane CG. A cutaneous disease caused by a new fungus Phialophora verrucosa. J Cutan Dis. 1915. 33:840-6.
Castro RM, Castro LG. On the priority of description of chromomycosis. Mykosen. 1987 Sep. 30(9):397-403. [QxMD MEDLINE Link].
Hoffman WH. Die Chromoblastomykose in Kuba. Arch Schiffs u Tropen Hyg. 1928. 32:485-7.
Pedroso A, Gomes JM. 4 casos de dermatite verrucosa produzida pela Phialophora verrucosa. Ann Paulistas de Medicina e Cirurgia. 1920. 11:53-61.
Brumpt E. Prés de Parasitologie. 3rd ed. Paris, France: Masson; 1922. 1105.
Negroni R. Estudio del primer caso argentino de cromomicosis, Fonsecaea (Negroni) pedrosoi (Brumpt) 1921. Rev Inst Bacteriol. 1936. 7:419-26.
Rippon JW. Chromoblastomycosis and related dermal infections caused by dematiaceous fungi. Medical Mycology. The Pathogenic Fungi and the Pathogenic Actinomycetes. 2nd ed. Philadelphia, Pa: WB Saunders; 1982. 249-76.
Lacaz CS, Porto E, Martins JEC. Fungos, actinomicetos e algas de interesse medico. Micologia Medica. 8th ed. Sao Paulo, Brazil: Sarvier; 1991. 373-86.
South DA, Brass C, Stevens DA. Chromohyphomycosis. Treatment wit ketoconazole. Arch Dermatol. 1981 May. 117(5):311-2. [QxMD MEDLINE Link].
Naka W, Harada T, Nishikawa T, Fukushiro R. A case of chromoblastomycosis: with special reference to the mycology of the isolated Exophiala jeanselmei. Mykosen. 1986 Oct. 29(10):445-52. [QxMD MEDLINE Link].
Barba-Gomez JF, Mayorga J, McGinnis MR, Gonzalez-Mendoza A. Chromoblastomycosis caused by Exophiala spinifera. J Am Acad Dermatol. 1992 Feb. 26(2 Pt 2):367-70. [QxMD MEDLINE Link].
Queiroz-Telles F, Purim KS, Fillus JN, et al. Itraconazole in the treatment of chromoblastomycosis due to Fonsecaea pedrosoi. Int J Dermatol. 1992 Nov. 31(11):805-12. [QxMD MEDLINE Link].
Padhye AA, Hampton AA, Hampton MT, Hutton NW, Prevost-Smith E, Davis MS. Chromoblastomycosis caused by Exophiala spinifera. Clin Infect Dis. 1996 Feb. 22(2):331-5. [QxMD MEDLINE Link].
Piepenbring M, Caceres Mendez OA, Espino Espinoza AA, Kirschner R, Schofer H. Chromoblastomycosis caused by Chaetomium funicola: a case report from Western Panama. Br J Dermatol. 2007 Nov. 157(5):1025-9. [QxMD MEDLINE Link].
Conant NF. The occurrence of a human pathogenic fungus as a saprophyte in nature. Mycologia. 1937. 29:597-8.
Zeppenfeldt G, Richard-Yegres N, Yegres F. Cladosporium carrionii: hongo dimorfico en cactaceas de la zona endemica para la cromomicosis en Venezuela. Rev Iberoam Micol. 1994. 11:61-3.
Najafzadeh MJ, Sun J, Vicente V, Xi L, van den Ende AH, de Hoog GS. Fonsecaea nubica sp. nov, a new agent of human chromoblastomycosis revealed using molecular data. Med Mycol. 2010 Mar 22. [QxMD MEDLINE Link].
You Z, Yang X, Yu J, Zhang J, Ran Y. Chromoblastomycosis Caused by Fonsecaea nubica: First Report in Northern China and Literature Review. Mycopathologia. 2019 Feb. 184 (1):97-105. [QxMD MEDLINE Link].
Badali H, Bonifaz A, Barrón-Tapia T, Vázquez-González D, Estrada-Aguilar L, Cavalcante Oliveira NM, et al. Rhinocladiella aquaspersa, proven agent of verrucous skin infection and a novel type of chromoblastomycosis. Med Mycol. 2010 Jan 29. [QxMD MEDLINE Link].
Silva CM, da Rocha RM, Moreno JS, et al. [The coconut babaçu (Orbignya phalerata martins) as a probable risk of human infection by the agent of chromoblastomycosis in the State of Maranhão, Brazil]. Rev Soc Bras Med Trop. 1995 Jan-Mar. 28(1):49-52. [QxMD MEDLINE Link].
Salgado CG, da Silva JP, Diniz JA, et al. Isolation of Fonsecaea pedrosoi from thorns of Mimosa pudica, a probable natural source of chromoblastomycosis. Rev Inst Med Trop Sao Paulo. 2004 Jan-Feb. 46(1):33-6. [QxMD MEDLINE Link].
Martinez EC, Rey Valeiron C, Yegres F, Reyes R. [The goat: approach to an animal model in human chromomycosis]. Invest Clin. 2005 Jun. 46(2):131-8. [QxMD MEDLINE Link].
Tsuneto LT, Arce-Gomez B, Petzl-Erler ML, Queiroz-Telles F. HLA-A29 and genetic susceptibility to chromoblastomycosis. J Med Vet Mycol. 1989. 27(3):181-5. [QxMD MEDLINE Link].
Brygoo ER, Destombes P. Epidemiologie de la chromoblastomycose humaine. Bull Inst Pasteur. 1975. 74:219-43.
Nishimoto K. Chromomycosis in Japan. Ann Soc Belg Med Trop. 1981 Sep. 61(3):405-12. [QxMD MEDLINE Link].
Berger L, Langeron M. Sur un type noveau de chromomycose observé au Canada (Torula bergeri n. sp). Ann Parasit Hum Comp. 1949. 24:574-99.
Putkonen T. [Chromomycosis in Finland. The possible role of the Finnish sauna in its spreading]. Hautarzt. 1966 Nov. 17(11):507-9. [QxMD MEDLINE Link].
Sonck CE. Chromomycosis in Finland. Dermatology. 1975. 19:189-93.
Yang CS, Chen CB, Lee YY, Yang CH, Chang YC, Chung WH, et al. Chromoblastomycosis in Taiwan: A report of 30 cases and a review of the literature. Med Mycol. 2018 Jun 1. 56 (4):395-405. [QxMD MEDLINE Link].
Pradhan SV, Talwar OP, Ghosh A, Swami RM, Shiva Raj KC, Gupta S. Chromoblastomycosis in Nepal: a study of 13 cases. Indian J Dermatol Venereol Leprol. 2007 May-Jun. 73(3):176-8. [QxMD MEDLINE Link].
Xi L, Sun J, Lu C, et al. Molecular diversity of Fonsecaea (Chaetothyriales) causing chromoblastomycosis in southern China. Med Mycol. 2009 Feb. 47(1):27-33. [QxMD MEDLINE Link].
Chandran V, Sadanandan SM, Sobhanakumari K. Chromoblastomycosis in kerala, India. Indian J Dermatol Venereol Leprol. 2012 Nov-Dec. 78(6):728-33. [QxMD MEDLINE Link].
Marques GF, Masuda PY, Sousa JM, Barreto JA, Wachholz PA. Clinical and demographic profile of chromoblastomycosis in a referral service in the midwest of São Paulo state (Brazil). An Bras Dermatol. 2015 Jan-Feb. 90(1):140-2. [QxMD MEDLINE Link]. [Full Text].
Schieffelin JS, Garcia-Diaz JB, Loss GE Jr, Beckman EN, Keller RA, Staffeld-Coit C, et al. Phaeohyphomycosis fungal infections in solid organ transplant recipients: clinical presentation, pathology, and treatment. Transpl Infect Dis. 2014 Mar 17. [QxMD MEDLINE Link].
Salgado CG, da Silva MB, Yamano SS, Salgado UI, Diniz JA, da Silva JP. Cutaneous localized annular chromoblastomycosis. J Cutan Pathol. 2009 Feb. 36(2):257-61. [QxMD MEDLINE Link].
El Euch D, Mokni M, Haouet S, Trojjet S, Zitouna M, Ben Osman A. [Erythemato-squamous papular and atrophic plaque on abdomen: chromoblastomycosis due to Fonsecaea pedrosoi]. Med Trop (Mars). 2010 Feb. 70(1):81-3. [QxMD MEDLINE Link].
Sharma NL, Sharma VC, Mahajan V, Shanker V, Sarin S. Chromoblastomycosis with underlying osteolytic lesion. Mycoses. 2007 Nov. 50(6):517-9. [QxMD MEDLINE Link].
Krishna S, Shenoy MM, Pinto M, Saxena V. Two cases of axillary chromoblastomycosis. Indian J Dermatol Venereol Leprol. 2016 Jan 21. [QxMD MEDLINE Link].
França K, Villa RT, de Azevedo Bastos VR, Almeida AC, Massucatti K, Fukumaru D, et al. Auricular Chromoblastomycosis: A Case Report and Review of Published Literature. Mycopathologia. 2011 Feb 17. [QxMD MEDLINE Link].
Sharma A, Hazarika NK, Gupta D. Chromoblastomycosis in Sub-Tropical Regions of India. Mycopathologia. 2010 Jan 22. [QxMD MEDLINE Link].
Naveen KN, Naik AS, Shetty PC, Pai VV, Hanumanthayya K, Udupishastry D. Chromoblastomycosis presenting as a phagedenic ulcer on the face. Int J Dermatol. 2011 Sep 19. [QxMD MEDLINE Link].
Slesak G, Inthalad S, Strobel M, Marschal M, Hall M Jr, Newton PN. Chromoblastomycosis after a leech bite complicated by myiasis: a case report. BMC Infect Dis. 2011 Jan 12. 11:14. [QxMD MEDLINE Link]. [Full Text].
Rojas OC, González GM, Moreno-Treviño M, Salas-Alanis J. Chromoblastomycosis by Cladophialophora carrionii Associated with Squamous Cell Carcinoma and Review of Published Reports. Mycopathologia. 2015 Feb. 179(1-2):153-7. [QxMD MEDLINE Link].
Thomas E, Bertolotti A, Barreau A, Klisnick J, Tournebize P, Borgherini G, et al. From phaeohyphomycosis to disseminated chromoblastomycosis: A retrospective study of infections caused by dematiaceous fungi. Med Mal Infect. 2018 Jun. 48 (4):278-285. [QxMD MEDLINE Link].
Hagiya H, Maeda T, Kusakabe S, Kawasaki K, Hori Y, Kimura K, et al. A fatal case of Exophiala dermatitidis disseminated infection in an allogenic hematopoietic stem cell transplant recipient during micafungin therapy. J Infect Chemother. 2019 Jun. 25 (6):463-466. [QxMD MEDLINE Link].
Verma S, Verma GK, Singh G, Kanga A, Sharma V, Gautam N. Facial chromoblastomycosis in sub-Himalayan region misdiagnosed as cutaneous leishmaniasis: brief report and review of Indian literature. Dermatol Online J. 2012 Oct 15. 18(10):3. [QxMD MEDLINE Link].
Azevedo CM, Marques SG, Santos DW, Silva RR, Silva NF, Santos DA, et al. Squamous Cell Carcinoma Derived From Chronic Chromoblastomycosis in Brazil. Clin Infect Dis. 2015 Feb 13. [QxMD MEDLINE Link].
Wang J, Zhu M, Wang P. Chromoblastomycosis by Exophiala jeanselmei associated with squamous cell carcinoma. J Mycol Med. 2021 Mar. 31 (1):101105. [QxMD MEDLINE Link].
Campolina SS, Caligiorne RB, Rezende-Silva S, Hahn RC, De Hoog GS. A skin infection mimicking chromoblastomycosis by a Capnodialean fungus. Med Mycol. 2009 Feb. 47(1):81-5. [QxMD MEDLINE Link].
Bui AQ, Espana EM, Margo CE. Chromoblastomycosis of the conjunctiva mimicking melanoma of the ciliary body. Arch Ophthalmol. 2012 Dec 1. 130(12):1615-7. [QxMD MEDLINE Link].
Skupsky H, Junkins-Hopkins J. Counterfeit Pennies: Distinguishing Chromoblastomycosis From Phaeohyphomycotic Infections. Am J Dermatopathol. 2017 Jun. 39 (6):485-487. [QxMD MEDLINE Link].
Anjaneyan G, Jagadeesan S, Thomas J. Cytodiagnostic copper pennies in chromoblastomycosis. Indian Dermatol Online J. 2016 Mar-Apr. 7 (2):145-6. [QxMD MEDLINE Link].
Miranda MF, Silva AJ. Vinyl adhesive tape also effective for direct microscopy diagnosis of chromomycosis, lobomycosis, and paracoccidioidomycosis. Diagn Microbiol Infect Dis. 2005 May. 52(1):39-43. [QxMD MEDLINE Link].
Saxena AK, Jain S, Ramesh V, Singh A, Capoor MR. Chromoblastomycosis: Demonstration of abundant microorganisms on microscopy of a scaly crust following intralesional corticosteroids. J Eur Acad Dermatol Venereol. 2014 Feb 14. [QxMD MEDLINE Link].
Vidal MS. Estudo imunoquimco de um antigeno de Fonsecaea pedrosoi e padronizao de teiicas sorologicas para cromoblastomicose causada por este fungo. Sao Paulo, Brazil: University of Sao Paulo; 2002.
Oberto-Perdigon L, Romero H, Perez-Blanco M, Apitz-Castro R. [An ELISA test for the study of the therapeutic evolution of chromoblastomycosis by Cladophialophora carrionii in the endemic area of Falcon State, Venezuela]. Rev Iberoam Micol. 2005 Mar. 22(1):39-43. [QxMD MEDLINE Link].
de Andrade TS, Cury AE, de Castro LG, Hirata MH, Hirata RD. Rapid identification of Fonsecaea by duplex polymerase chain reaction in isolates from patients with chromoblastomycosis. Diagn Microbiol Infect Dis. 2007 Mar. 57(3):267-72. [QxMD MEDLINE Link].
Najafzadeh MJ, Sun J, Vicente VA, de Hoog GS. Rapid identification of fungal pathogens by rolling circle amplification using Fonsecaea as a model. Mycoses. 2011 Sep. 54(5):e577-82. [QxMD MEDLINE Link].
Ogawa MM. Cromoblastomicose: Teraplicas e alternativos linfocintilograpicas. Sao Paulo, Brazil: Tese de Mestrado, Escola Paulista de Medicina; 2001.
Salfelder K, de Liscano TR, Sauerteig E. Atlas of Fungal Pathology. Kluwer/Dordrecht; 1990. 145-50.
Jawitz RS, Calder KB, Turner LM, Schlauder S, Morgan MB. Cryptic "chromo-fibroma". Am J Dermatopathol. 2007 Dec. 29(6):573-5. [QxMD MEDLINE Link].
Queiroz-Telles F, Esterre P, Perez-Blanco M, Vitale RG, Salgado CG, Bonifaz A. Chromoblastomycosis: an overview of clinical manifestations, diagnosis and treatment. Med Mycol. 2009 Feb. 47(1):3-15. [QxMD MEDLINE Link].
Antonello VS, Silva MC, Cambruzzi E, Kliemann DA, Santos BR, Queiroz-Telles F. Treatment of severe chromoblastomycosis with itraconazole and 5-flucytosine association. Rev Inst Med Trop Sao Paulo. 2010 Dec. 52(6):329-31. [QxMD MEDLINE Link].
Restrepo A, Gonzalez A, Gomez I, Arango M, de Bedout C. Treatment of chromoblastomycosis with itraconazole. Ann N Y Acad Sci. 1988. 544:504-16. [QxMD MEDLINE Link].
Graybill JR. Future directions of antifungal chemotherapy. Clin Infect Dis. 1992 Mar. 14 Suppl 1:S170-81. [QxMD MEDLINE Link].
Bonifaz A, Carrasco-Gerard E, Saul A. Chromoblastomycosis: clinical and mycologic experience of 51 cases. Mycoses. 2001. 44(1-2):1-7. [QxMD MEDLINE Link].
Zhang J, Xi L, Lu C, et al. Successful treatment for chromoblastomycosis caused by Fonsecaea monophora: a report of three cases in Guangdong, China. Mycoses. 2009 Mar. 52(2):176-81. [QxMD MEDLINE Link].
Shen XC, Dai XN, Xie ZM, Li P, Lu S, Li JH, et al. A Case of Chromoblastomycosis Caused by Fonsecaea pedrosoi Successfully Treated by Oral Itraconazole Together with Terbinafine. Dermatol Ther (Heidelb). 2020 Apr. 10 (2):321-327. [QxMD MEDLINE Link].
Pradinaud R, Bolzinger T. Treatment of chromoblastomycosis. J Am Acad Dermatol. 1991 Nov. 25(5 Pt 1):869-70. [QxMD MEDLINE Link].
Esterre P, Inzan CK, Ramarcel ER, et al. Treatment of chromomycosis with terbinafine: preliminary results of an open pilot study. Br J Dermatol. 1996 Jun. 134 Suppl 46:33-6; discussion 40. [QxMD MEDLINE Link].
Keating GM. Posaconazole. Drugs. 2005. 65(11):1553-67; discussion 1568-9. [QxMD MEDLINE Link].
Belda W Jr, Criado PR, Passero LFD. Successful treatment of chromoblastomycosis caused by Fonsecaea pedrosoi using imiquimod. J Dermatol. 2020 Apr. 47 (4):409-412. [QxMD MEDLINE Link].
Lyon JP, Pedroso e Silva Azevedo Cde M, Moreira LM, de Lima CJ, de Resende MA. Photodynamic antifungal therapy against chromoblastomycosis. Mycopathologia. 2011 Oct. 172(4):293-7. [QxMD MEDLINE Link].
Hu Y, Huang X, Lu S, Hamblin MR, Mylonakis E, Zhang J, et al. Photodynamic Therapy Combined with Terbinafine Against Chromoblastomycosis and the Effect of PDT on Fonsecaea monophora In Vitro. Mycopathologia. 2015 Feb. 179(1-2):103-9. [QxMD MEDLINE Link]. [Full Text].
Yang Y, Hu Y, Zhang J, Li X, Lu C, Liang Y, et al. A refractory case of chromoblastomycosis due to Fonsecaea monophora with improvement by photodynamic therapy. Med Mycol. 2012 Feb 7. [QxMD MEDLINE Link].
Huang X, Han K, Wang L, Peng X, Zeng K, Li L. Successful treatment of chromoblastomycosis using ALA-PDT in a patient with leukopenia. Photodiagnosis Photodyn Ther. 2019 Feb 12. [QxMD MEDLINE Link].
Kinbara T, Fukushiro R, Eryu Y. Chromomycosis--report of two cases successfully treated with local heat therapy. Mykosen. 1982 Dec. 25(12):689-94. [QxMD MEDLINE Link].
Tagami H, Ginoza M, Imaizumi S, Urano-Suehisa S. Successful treatment of chromoblastomycosis with topical heat therapy. J Am Acad Dermatol. 1984 Apr. 10(4):615-9. [QxMD MEDLINE Link].
da Glória Teixeira de Sousa M, Júnior WB, Spina R, Lota PR, Valente NS, Brown GD, et al. Topical application of Imiquimod as a treatment for Chromoblastomycosis. Clin Infect Dis. 2014 Mar 14. [QxMD MEDLINE Link].
Bassas-Vila J, Fuente MJ, Guinovart R, Ferrándiz C. Chromoblastomycosis: response to combination therapy with cryotherapy and terbinafine. Actas Dermosifiliogr. 2014 Mar. 105(2):196-8. [QxMD MEDLINE Link].
Pimentel ER, Castro LG, Cuce LC, Sampaio SA. Treatment of chromomycosis by cryosurgery with liquid nitrogen: a report on eleven cases. J Dermatol Surg Oncol. 1989 Jan. 15(1):72-7. [QxMD MEDLINE Link].
Ameen M. Managing chromoblastomycosis. Trop Doct. 2010 Apr. 40(2):65-7. [QxMD MEDLINE Link].
Badali H, Fernández-González M, Mousavi B, Illnait-Zaragozi MT, González-Rodríguez JC, de Hoog GS, et al. Chromoblastomycosis due to Fonsecaea pedrosoi and F. monophora in Cuba. Mycopathologia. 2013 Mar 8. [QxMD MEDLINE Link].
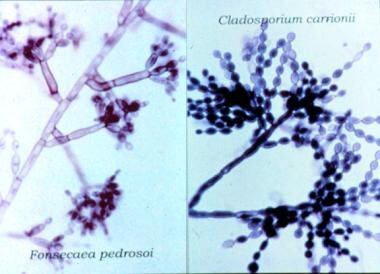 Micromorphology of Cladosporium carrionii (left) and Fonsecaea pedrosoi (right), the 2 most commonly isolated agents in chromoblastomycosis.
Micromorphology of Cladosporium carrionii (left) and Fonsecaea pedrosoi (right), the 2 most commonly isolated agents in chromoblastomycosis.
 Culture of Fonsecaea pedrosoi on Sabouraud agar. The black velvety colony has the same macroscopic appearance as the colonies of other chromoblastomycosis-causing agents (eg, Cladosporium carrionii, Fonsecaea compacta, Phialophora verrucosa, Rhinocladiella aquaspersa, Exophiala species).
Culture of Fonsecaea pedrosoi on Sabouraud agar. The black velvety colony has the same macroscopic appearance as the colonies of other chromoblastomycosis-causing agents (eg, Cladosporium carrionii, Fonsecaea compacta, Phialophora verrucosa, Rhinocladiella aquaspersa, Exophiala species).
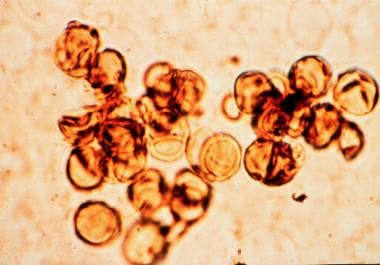
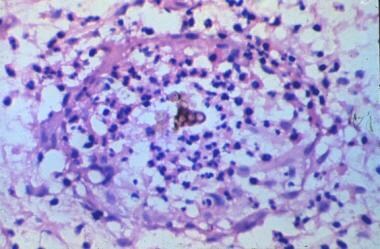 Hematoxylin and eosin–stained section shows typical sclerotic cells inside an abscess. Sclerotic cells present as round, thick-walled, cigar-colored structures.
Hematoxylin and eosin–stained section shows typical sclerotic cells inside an abscess. Sclerotic cells present as round, thick-walled, cigar-colored structures.