Mannheimer SB, Soave R. Protozoal infections in patients with AIDS. Cryptosporidiosis, isosporiasis, cyclosporiasis, and microsporidiosis. Infect Dis Clin North Am. 1994 Jun. 8(2):483-98. [QxMD MEDLINE Link].
Stark D, Barratt JL, van Hal S, Marriott D, Harkness J, Ellis JT. Clinical significance of enteric protozoa in the immunosuppressed human population. Clin Microbiol Rev. 2009 Oct. 22(4):634-50. [QxMD MEDLINE Link]. [Full Text].
Murray P, Rosenthal K, Pfaller M. Intestinal and Urogenital protozoa. Medical Microbiology. 7th edition. 2013. 745-758.
Huang P, Weber JT, Sosin DM, Griffin PM, Long EG, Murphy JJ, et al. The first reported outbreak of diarrheal illness associated with Cyclospora in the United States. Ann Intern Med. 1995 Sep 15. 123(6):409-14. [QxMD MEDLINE Link].
Carter RJ, Guido F, Jacquette G, Rapoport M. Outbreak of cyclosporiasis at a country club -- New York, 1995. : 45th Annual Epidemic Intelligence Service (EIS) Conference. Atlanta, Georgia: US Department of Health and Human Services, Public Health Service April 1996:58;
Herwaldt BL, Ackers ML. An outbreak in 1996 of cyclosporiasis associated with imported raspberries. The Cyclospora Working Group. N Engl J Med. 1997 May 29. 336(22):1548-56. [QxMD MEDLINE Link].
Ho AY, Lopez AS, Eberhart MG, et al. Outbreak of cyclosporiasis associated with imported raspberries, Philadelphia, pennsylvania, 2000. Emerg Infect Dis. 2002 Aug. 8(8):783-8. [QxMD MEDLINE Link]. [Full Text].
CDC. From the Centers for Disease Control and Prevention. Outbreaks of cyclosporiasis--United States, 1997. JAMA. 1997 Jun 11. 277(22):1754. [QxMD MEDLINE Link].
CDC. From the Centers for Disease Control and Prevention. Update: outbreaks of cyclosporiasis--1997. JAMA. 1997 Jul 9. 278(2):108. [QxMD MEDLINE Link].
CDC. From the Centers for Disease Control and Prevention. Update: outbreaks of cyclosporiasis--United States, 1997. JAMA. 1997 Jun 18. 277(23):1838. [QxMD MEDLINE Link].
CDC. From the Centers for Disease Control. Outbreak of cyclosporiasis-- Northern Virginia-Washington, DC-Baltimore, Maryland, metropolitan area, 1997. JAMA. 1997 Aug 20. 278(7):538-9. [QxMD MEDLINE Link].
Hoang LM, Fyfe M, Ong C, et al. Outbreak of cyclosporiasis in British Columbia associated with imported Thai basil. Epidemiol Infect. 2005 Feb. 133(1):23-7. [QxMD MEDLINE Link].
Heilpern KL, Wald M. Update on emerging infections: news from the Centers for Disease Control and Prevention. Outbreak of cyclosporiasis associated with snow peas--Pennsylvania, 2004. Ann Emerg Med. 2005 May. 45(5):529-31. [QxMD MEDLINE Link].
Centers for Disease Control and Prevention (CDC). outbreaks of cyclosporiasis--United States, June-August 2013. MMWR Morb Mortal Wkly Rep. 2013 Nov 1. 62(43):862. [QxMD MEDLINE Link].
CDC. Parasites - Cyclosporiasis (Cyclospora Infection). Centers for Disease Control and Prevention. Available at https://www.cdc.gov/parasites/cyclosporiasis/outbreaks/index.html. 2021 Aug 26; Accessed: November 10, 2022.
Almeria S, Shipley A. Detection of Cyclospora cayetanensis on bagged pre-cut salad mixes within their shelf-life and after sell by date by the U.S. food and drug administration validated method. Food Microbiol. 2021 Sep. 98:103802. [QxMD MEDLINE Link].
Hall NB, Chancey RJ, Keaton AA, et al. Cyclosporiasis Epidemiologically Linked to Consumption of Green Onions: Houston Metropolitan Area, August 2017. J Food Prot. 2020 Jan 21. 326-30. [QxMD MEDLINE Link].
Increase in Reported cases of Cyclospora cayetanensis Infection, United States, Summer 2017. CDC Health Alert Network. Available at https://emergency.cdc.gov/han/han00405.asp. August 07, 2017; Accessed: August 8, 2017.
Chacin-Bonilla L. Epidemiology of Cyclospora cayetanensis: A review focusing in endemic areas. Acta Trop. 2010 Sep. 115(3):181-93. [QxMD MEDLINE Link].
Samie A, Guerrant RL, Barrett L, Bessong PO, Igumbor EO, Obi CL. Prevalence of intestinal parasitic and bacterial pathogens in diarrhoeal and non-diarroeal human stools from Vhembe district, South Africa. J Health Popul Nutr. 2009 Dec. 27(6):739-45. [QxMD MEDLINE Link]. [Full Text].
Blans MC, Ridwan BU, Verweij JJ, et al. Cyclosporiasis outbreak, Indonesia. Emerg Infect Dis. 2005 Sep. 11(9):1453-5. [QxMD MEDLINE Link].
Iqbal J, Hira PR, Al-Ali F, Khalid N. Cyclospora cayetanensis: first report of imported and autochthonous infections in Kuwait. J Infect Dev Ctries. 2011 May 28. 5(5):383-90. [QxMD MEDLINE Link].
Zhou Y, Lv B, Wang Q, Wang R, Jian F, Zhang L, et al. Prevalence and molecular characterization of Cyclospora cayetanensis, Henan, China. Emerg Infect Dis. 2011 Oct. 17(10):1887-90. [QxMD MEDLINE Link]. [Full Text].
Sifuentes-Osornio J, Porras-Cortés G, Bendall RP, Morales-Villarreal F, Reyes-Terán G, Ruiz-Palacios GM. Cyclospora cayetanensis infection in patients with and without AIDS: biliary disease as another clinical manifestation. Clin Infect Dis. 1995 Nov. 21(5):1092-7. [QxMD MEDLINE Link].
Zar FA, El-Bayoumi E, Yungbluth MM. Histologic proof of acalculous cholecystitis due to Cyclospora cayetanensis. Clin Infect Dis. 2001 Dec 15. 33(12):E140-1. [QxMD MEDLINE Link].
de Górgolas M, Fortés J, Fernández Guerrero ML. Cyclospora cayetanensis Cholecystitis in a patient with AIDS. Ann Intern Med. 2001 Jan 16. 134(2):166. [QxMD MEDLINE Link].
Richardson RF Jr, Remler BF, Katirji B, Murad MH. Guillain-Barré syndrome after Cyclospora infection. Muscle Nerve. 1998 May. 21(5):669-71. [QxMD MEDLINE Link].
Connor BA, Johnson EJ, Soave R. Reiter syndrome following protracted symptoms of Cyclospora infection. Emerg Infect Dis. 2001 May-Jun. 7(3):453-4. [QxMD MEDLINE Link]. [Full Text].
Visvesvara GS, Moura H, Kovacs-Nace E, Wallace S, Eberhard ML. Uniform staining of Cyclospora oocysts in fecal smears by a modified safranin technique with microwave heating. J Clin Microbiol. 1997 Mar. 35(3):730-3. [QxMD MEDLINE Link]. [Full Text].
McHardy IH, Wu M, Shimizu-Cohen R, Couturier MR, Humphries RM. Detection of intestinal protozoa in the clinical laboratory. J Clin Microbiol. 2014 Mar. 52(3):712-20. [QxMD MEDLINE Link]. [Full Text].
Bourée P, Lancon A, Bisaro F, Bonnot G. Six human cyclosporiasis: with general review. J Egypt Soc Parasitol. 2007 Aug. 37(2):349-60. [QxMD MEDLINE Link].
Verdier RI, Fitzgerald DW, Johnson WD Jr, Pape JW. Trimethoprim-sulfamethoxazole compared with ciprofloxacin for treatment and prophylaxis of Isospora belli and Cyclospora cayetanensis infection in HIV-infected patients. A randomized, controlled trial. Ann Intern Med. 2000 Jun 6. 132(11):885-8. [QxMD MEDLINE Link].
Diaz E, Mondragon J, Ramirez E, Bernal R. Epidemiology and control of intestinal parasites with nitazoxanide in children in Mexico. Am J Trop Med Hyg. 2003 Apr. 68(4):384-5. [QxMD MEDLINE Link].
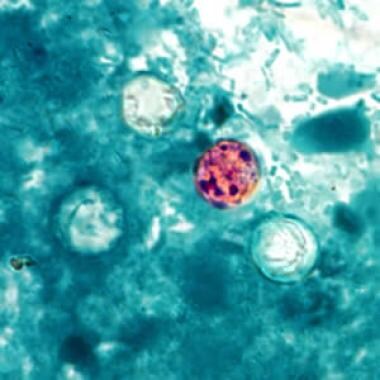 Oocysts of C cayetanensis stained with modified acid-fast stain. Note the variability of staining in the four oocysts. Courtesy of the CDC (http://phil.cdc.gov/phil/home.asp).
Oocysts of C cayetanensis stained with modified acid-fast stain. Note the variability of staining in the four oocysts. Courtesy of the CDC (http://phil.cdc.gov/phil/home.asp).
 Oocyst of C cayetanensis viewed under UV microscopy. Courtesy of the CDC (http://phil.cdc.gov/phil/home.asp).
Oocyst of C cayetanensis viewed under UV microscopy. Courtesy of the CDC (http://phil.cdc.gov/phil/home.asp).








