ectopic pregnancy
Also found in: Dictionary, Thesaurus, Legal, Acronyms, Encyclopedia, Wikipedia.
Ectopic Pregnancy
Definition
Description
Causes and symptoms
- Endometriosis. A condition in which the tissue that normally lines the uterus is found outside the uterus, and can block a fallopian tube.
- Exposure to diethylsilbestrol (DES) as a fetus. If a woman's mother took DES (a synthetic version of the hormone estrogen) during pregnancy, the woman may have abnormalities in her fallopian tubes that can make ectopic pregnancy more likely.
- Taking hormones. Estrogen and progesterone are hormones that regulate the menstrual cycle and may be in medications prescribed by a doctor for birth control or other reasons. Taking these hormones can affect the interior lining of the fallopian tubes and slow the movement of the fertilized egg down the tube. Women who become pregnant in spite of taking some progesterone-only contraceptives have a greater chance of an ectopic pregnancy. Ectopic pregnancy is also more likely when the ovaries are artificially stimulated with hormones to produce eggs for in vitro fertilization (a procedure in which eggs are taken from a woman's body, fertilized, and then placed in the uterus in an attempt to conceive a child).
- Use of an intrauterine device (IUD). These contraceptive devices are designed to prevent fertilized eggs from becoming implanted in the uterus, but they have only a minimal effect on preventing ectopic pregnancies. Therefore, if a woman becomes pregnant while using an IUD for contraception, the fertilized egg is more likely to be implanted someplace other than the uterus. For example, among women who become pregnant while using a progesterone-bearing IUD, about 15% have ectopic pregnancies.
- Surgery on a fallopian tube. The risk of ectopic pregnancy can be as high as 60% after undergoing elective tubal sterilization, a procedure in which the fallopian tubes are severed to prevent pregnancy. Women who have successful surgery to reverse the procedure are also more likely to have an ectopic pregnancy.
Early symptoms
Later symptoms
Diagnosis
Treatment
Medical
Surgical
Alternative treatment
Key terms
Prognosis
Prevention
Resources
Organizations
pregnancy
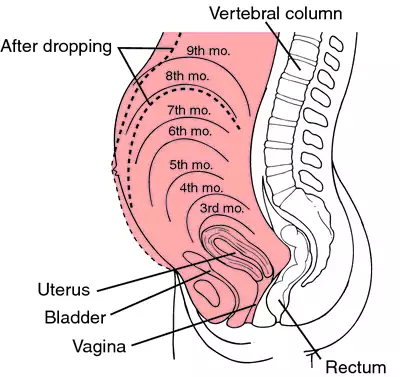
[preg´nan-se]Other signs of pregnancy include softening of the cervix and filling of the cervical canal with a plug of mucus. Early in labor this plug is expelled and there is slight bleeding; expulsion of the mucous plug is known as show and indicates the beginning of cervical dilatation. chadwick's sign of pregnancy refers to a bluish color of the vagina which is a result of increased blood supply to the area.
When the abdominal wall becomes stretched there may be a breaking down of elastic tissues, resulting in depressed areas in the skin which are smooth and reddened. These markings are called striae gravidarum. In subsequent pregnancies the old striae appear as whitish streaks and frequently do not disappear completely.
There are several fairly accurate laboratory tests for pregnancy; all are designed to detect human chorionic gonadotropin (hCG), a hormone produced by living chorionic placental tissue and evident in the blood and urine of pregnant women. See also pregnancy tests.
There is now less emphasis on severe restriction of the mother's dietary intake to maintain a limited weight gain. The average gain is about 28 lb during pregnancy, and either starvation diets or forced feedings can be unhealthy for the mother and hazardous for the fetus. Ideally, the mother should achieve normal weight before she becomes pregnant because obesity increases the possibility of eclampsia and other serious complications of pregnancy. Mothers who are underweight are more likely to deliver immature babies who, by virtue of their physiologic immaturity, are more likely to suffer from birth defects, hyaline membrane disease, and other developmental disorders of the newborn.
Other factors affecting the fetus include certain drugs taken by the mother during pregnancy. A well-known example is thalidomide, which inhibits the growth of the extremities of the fetus, resulting in gross deformities. Many drugs, including prescription as well as nonprescription medications, are now believed to be capable of causing fetal abnormalities. In addition, consumption of alcohol during pregnancy may result in fetal alcohol syndrome. Most health care providers recommend that all drugs be avoided during pregnancy except those essential to the control of disease in the mother.
Diseases that increase the risk of obstetrical complications include diabetes, heart disease, hypertension, kidney disease, and anemia. rubella (German measles) can be responsible for many types of birth defects, particularly if the mother contracts it in the first 3 months of pregnancy. Sexually transmitted diseases can have tragic effects on the baby, even though the symptoms in the mother are minor at the time of pregnancy. syphilis is particularly dangerous because it is one of the few diseases that can be transmitted to the fetus in utero. The baby is either stillborn or born infected, and rarely escapes physical or mental defects or both. Successful treatment of the mother before the fifth month of pregnancy will prevent infection in the infant.
During the birth process the infant may be infected with gonorrhea as it passes through the birth canal. Gonorrheal infection of the eyes can cause blindness. herpes simplex Type II involving the genitals of the mother can also be transmitted to the infant at birth. The mortality and morbidity rates for such infected infants are high.
The age of the mother is also an important factor in the well-being of the fetus. The mortality and morbidity rate for infants born of mothers below age 15 and above 40 are higher than for those of mothers between these ages.
Recently developed tests to monitor fetal health have taken much of the guesswork out of predicting the chances of survival and health status of the fetus after birth. Such tests and evaluation techniques include amniocentesis, chemical and hormonal assays, biophysical profiles, testing for alpha-fetoprotein, ultrasound examinations, electronic surveillance of fetal vital signs and reaction to uterine contractions, and analyses of the infant's blood during labor.
On the first prenatal visit the patient's medical history is taken in considerable detail, including any diseases or operations she has had, the course of previous pregnancies, if any, and whether there is a family history of multiple births or of diabetes mellitus or other chronic diseases. The first visit also includes a thorough physical examination and measurement of the pelvis. Blood samples are taken for screening for rubella and sexually transmitted diseases such as syphilis, hepatitis B, chlamydiosis, infection by the human immunodeficiency virus, and other conditions. A complete blood count is also needed. Urine is tested for albumin and sugar and examined microscopically. On subsequent visits the patient brings a urine specimen, collected upon arising that morning, to be tested for albumin and glucose. At each prenatal visit her blood pressure is taken and recorded and she is weighed. In the second trimester, when the uterus becomes an abdominal organ, the height of the fundus is measured at each visit. After the sixth month a rule such as mcdonald's rule can be applied to assess fetal growth.
Patients who are considered high-risk mothers usually are sent to a specialist and the infant is delivered at a regional hospital where sophisticated monitoring equipment and laboratory tests are available, and specially trained personnel can attend to the needs of the mother and her infant.
A visit to a dentist early in pregnancy is a good idea to forestall any possibility of infection arising from tooth decay. Pregnancy does not encourage tooth decay. Hemorrhoids sometimes occur in pregnancy because of pressure from the enlarged uterus on the veins in the rectum. The health care provider should be consulted for treatment. varicose veins also result from pressure of the uterus, which restricts the flow of blood from the legs and feet. Lying flat with the feet raised on a pillow several times a day will help relieve swelling and pain in the legs. In more difficult cases the health care provider may prescribe an elastic bandage or support stockings.
Backache during pregnancy is caused by the heavy abdomen pulling on muscles that are not normally used, and can be relieved by rest, sensible shoes, and good posture. Swelling of the feet and ankles usually is relieved by rest and by remaining off the feet for a day or two. If the swelling does not disappear, the health care provider should be informed since it may be an indication of a more serious complication.
Shortness of breath is common in the later stages of pregnancy. If at any time it becomes so extreme that the woman cannot climb a short flight of stairs without discomfort, the health care provider should be consulted. If a mild shortness of breath interferes with sleep, lying in a half-sitting position, supported by several pillows, may help.
The more serious complications of pregnancy include pyelitis, hyperemesis gravidarum, eclampsia, and placenta previa and abruptio placentae.
In a tubal pregnancy a spontaneous abortion may occur, but more often the fetus will grow to a size large enough to rupture the tube. This is an emergency situation requiring immediate treatment. The symptoms of such a tubal rupture are vaginal bleeding and severe pain in one side of the abdomen. Prompt surgery is necessary to remove the damaged tube and the fetus, and to stop the bleeding. Fortunately, the removal of one tube usually leaves the other one intact, so that future pregnancy is possible. Patients who are Rh-negative should be given Rh0 (D) immune globulin (RhoGAM) after ectopic pregnancy for isoimmunization protection in future pregnancies.
ec·top·ic preg·nan·cy
ectopic pregnancy
ectopic pregnancy
Ectopic gestation Obstetrics The implantation of a fertilized outside of the uterus–eg, fallopian tube, ovary, peritoneum, and other tissues not designed to accommodate the vasculature required by a growing fetus Clinical Lower abdominal pain, vomiting, amenorrhea Management Surgeryec·top·ic preg·nan·cy
(ek-top'ik preg'năn-sē)Synonym(s): eccyesis.
ectopic pregnancy
Symptoms
Early complaints are consistent with those of a normal pregnancy (i.e., amenorrhea, breast tenderness, nausea). Pregnancy test results are positive owing to the presence of human chorionic gonadotropin (hCG) in blood and urine. Signs and symptoms arise as the growing embryo distends the fallopian tube; associated complaints include intermittent, unilateral, colicky abdominal pain. Complaints associated with tubal rupture include sharp unilateral pelvic or lower abdominal pain; orthostatic dizziness and vertigo or syncope; and referred shoulder pain related to peritoneal irritation from abdominal bleeding (hemoperitoneum). Signs of hypovolemic shock may indicate extensive abdominal bleeding. Vaginal bleeding, typically occurring after the onset of pain, is the result of decidual sloughing.
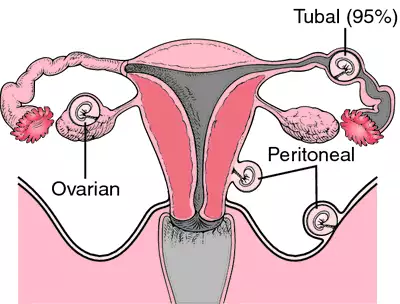
Locations
Abdominal: The incidence of pregnancy in the abdominal cavity with the conceptus attached to an abdominal organ is between 1:3000 and 1:4000 births. Ovarian: Conception and implantation within the ovary itself occurs in approximately 1 in 7,000 to 1 in 50,000 pregnancies. Tubal: Ninety to 95% of ectopic pregnancies occur in the fallopian tube; of these, 78% become implanted in the uterine ampulla, 12% in the isthmus, and 2% to 3% in the interstices.
Diagnosis
Transabdominal or transvaginal pelvic ultrasonography is used to identify the location of the pregnancy. It has also largely replaced culdocentesis for confirmation of hemoperitoneum.
Treatment
An operative approach is most common. Laparoscopy and linear laser salpingostomy can be used to excise early ectopic implantations; healing is by secondary intention. Segmental resection allows salvage and later reconstruction of the affected tube. Salpingectomy is reserved for cases in which tubal damage is so extensive that reanastomosis is not possible. Methotrexate has been used successfully to induce dissolution of unruptured tubal masses less than 3.5 cm. Posttreatment monitoring includes serial quantitative b-hCG levels, to be certain that the pregnancy has ended.
Patient care
Preoperative: The patient is assessed for pain and shock. Vital signs are monitored and oxygen administration by nonrebreather mask is started. An IV fluid infusion via a large-bore cannula is started and blood is drawn to type and cross (including Rh-compatibility) for potential transfusion. Medications (including RhoGAM if the patient is Rh negative) may be prescribed and administered and the patient's response evaluated. The patient's and family's wishes regarding religious rites for the products of conception are determined. Both patient and family are encouraged to express their feelings of fear, loss, and grief. Information regarding the condition and the need for surgical intervention is clarified.
Postoperative: Vital signs are monitored until stable, incisional dressings are inspected, vaginal bleeding is assessed, and the patient's physical and emotional reactions to the surgery are evaluated. Prescribed analgesics and other medications are administered, and the patient evaluated for desired and adverse effects. The grieving process is anticipated, and both the patient and family are referred for further counseling as needed.
ectopic pregnancy
A dangerous complication of pregnancy in which the fertilized egg (ovum) becomes implanted in an abnormal site, such as the FALLOPIAN TUBE or in the pelvis or abdomen, instead of in the womb lining. The great danger is severe, and sometimes life-threatening, bleeding (haemorrhage). Treatment is by urgent operation to remove the growing embryo. This is now mainly done by laparoscopic surgery.Ectopic Pregnancy
| DRG Category: | 777 |
| Mean LOS: | 2.3 days |
| Description: | MEDICAL: Ectopic Pregnancy |
An ectopic pregnancy is an implantation of the blastocyst (a solid mass of cells formed by rapid mitotic division of the zygote that eventually form the embryo) in a site other than the endometrial lining of the uterus. It is the leading cause of maternal death in the first trimester of pregnancy. In more than 95% of ectopic pregnancies, this implantation occurs somewhere in the fallopian tubes, hence the term “tubal pregnancy.” The fallopian tube lacks a submucosal layer, which allows the ovum to burrow through the epithelium. Fertilization occurs, and the zygote lies within the muscular wall of the tube, drawing its blood supply from maternal vessels. The ampullary portion of the tube is the most common site (80%), followed by the isthmic portion (12%) and the fimbria (5%). The cornual and interstitial regions of the tube have lower (2%) prevalence but a higher risk of mortality. Nontubal sites are more rare and include abdominal, ovarian, and cervical locations.
After the blastocyst implants in the tube, it begins to grow and can cause bleeding into the abdominal cavity. Eventually, the ovum becomes too large and the tube can rupture, causing further bleeding that can lead to shock and maternal death. Ectopic pregnancies occur in approximately 25 per 1,000 pregnancies, and non-European Americans have a 1.4 times increased risk over European Americans. Heterotopic pregnancies, in which there is an ectopic and a uterine pregnancy at the same time, occur at a rate of 1:10,000. The frequency of ectopic pregnancy has increased four-fold since 1970, owing to the increase in sexually transmitted infections (STIs), better diagnostic techniques, increased use of artificial reproductive technology, and increased use of tubal surgeries to treat infertility. Ectopic pregnancy accounts for 3% to 4% of all pregnancy-related deaths and reduces a woman’s chance of future pregnancy because of tubal damage; approximately one-third of women who experience an ectopic pregnancy subsequently give birth to a live infant. Hemorrhage, peritonitis, and infertility are the main complications.
Causes
The major cause of ectopic pregnancy is tubal damage, which can result from pelvic inflammatory disease, previous pelvic or tubal surgery, or endometriosis. Other causes may be hormonal factors that impede ovum transport and mechanically stop the forward movement of the egg in the tube, congenital anomalies of the tube, and a blighted ovum. Pelvic infections and STIs, specifically chlamydia and gonorrhea, are often involved. Other risk factors include smoking, diethylbestrol exposure, T-shaped uterus, certain intrauterine devices (IUDs), and a ruptured appendix.
Genetic considerations
No clear genetic contributions to susceptibility have been defined.
Gender, ethnic/racial, and life span considerations
In the United States, ectopic pregnancy is most often seen in non-European American women over age 35. Women of all ancestries over 40 have three times the likelihood of ectopic pregnancy as compared to their younger counterparts. Aging may result in progressive loss of myoelectrical activity responsible for moving the egg through the fallopian tube. Also, ectopic pregnancy often occurs in teens who have engaged in high-risk sexual practices that have resulted in frequent pelvic infections. African American teenagers and teenagers of other minority races have a mortality rate almost five times higher from ectopic pregnancy than white teenagers.
Global health considerations
In developing countries, deaths from ectopic pregnancy are 10 times higher than those reported in developed countries. Several reasons may contribute to this disparity, including increased prevalence due to untreated sexual transmitted infections and lack of prompt identification and intervention when an ectopic pregnancy occurs.
Assessment
History
Women in their childbearing years, including teens, should be evaluated for an ectopic pregnancy any time they are evaluated for abdominal pain, cramping, or vaginal bleeding. Elicit a history about the onset of menses, gynecological disorders, pattern of sexual practices and birth control, and past pregnancies. Patients with an ectopic pregnancy often have some history of tubular damage as a result of infections or endometriosis. They may also have had tubal surgeries. Often, patients describe a history of using an IUD, and some may report a history of infertility. Question the patient about her last menstrual period to determine the onset, duration, amount of bleeding, and whether it was a “normal” period for her. This description is important because although amenorrhea may be present in many cases of ectopic pregnancy, uterine bleeding that occurs with ectopic pregnancy may be mistaken for a menstrual period. In addition to amenorrhea, the patient may exhibit other signs of pregnancy, such as breast tenderness, nausea, and fatigue.
Physical examination
The most common symptoms include abdominal pain, amenorrhea, and vaginal bleeding. An undocumented ectopic pregnancy is a life-threatening emergency. Assess vaginal bleeding for the amount, color, and odor; if none is noted, bleeding may be concealed. Bleeding can occur as vaginal spotting, as a “slow leak,” or as a massive hemorrhage depending on the gestational age and whether the tube has ruptured. Usually, the bleeding is slow, and the abdomen can become rigid and tender. Sometimes, vaginal bleeding is present with the death of the embryo. If internal hemorrhage is profuse, the woman experiences signs and symptoms of hypovolemic shock (restlessness, agitation, confusion, cold and clammy skin, increased respirations and heart rate, delayed capillary blanching, hypotension).
Evaluate the patient’s pain; it can range from a feeling of fullness in the rectal area and abdominal cramping to excruciating pain. Often, the pain is one-sided and increases when the cervix is moved during a vaginal examination. Some women do not feel any pain until the tube is about to rupture, usually at the third month of gestation. If the tube ruptures, the woman experiences sharp, one-sided, lower abdominal pain and syncope. The pain may radiate to the shoulders and neck and is aggravated by situations that cause increased abdominal pressure, such as lifting or having a bowel movement.
Psychosocial
Often, the patient experiences anger, grief, guilt, and self-blame over the loss of the fetus. She may also be anxious about her ability to conceive in the future. Because much of her anxiety may stem from lack of information about her condition, assess her learning needs. Determine the ability of the father and other family members to cope and support the patient.
Diagnostic highlights
General Comments: Diagnosis is based on a positive pregnancy and inability to visualize the embryo in the uterus. Have a high index of suspicion for any female patient in her reproductive years who reports abdominal pain, cramping, or vaginal bleeding. All these females should be screened for ectopic pregnancy.
| Test | Normal Result | Abnormality With Condition | Explanation |
|---|---|---|---|
| Transvaginal ultrasonography | Intrauterine gestational sac is visualized | Unable to visualize intrauterine sac | This result, combined with a positive pregnancy test (elevated hCG), confirms the diagnosis |
| Human chorionic gonadotropin (hCG) | Normally is not present in nonpregnant women | The level is above the discriminatory zone of 1,500 mIU | hCG doubles every 2 days during the first 40 days of pregnancy; failure to do so is evidence of abnormality |
| Progesterone level (not accurate if fertility drugs were used) | > 25 ng/L | < 5 ng/L (values between 5 and 25 are inconclusive) | Progesterone increases with normal pregnancy |
Other Tests: Laparoscopic examination of the abdominal cavity (used only in confusing cases), color flow Doppler ultrasound (used in cases when the gestational sac is questionably empty), Rh antibody screen and blood type, complete blood count and coagulation studies, culdocentesis
Primary nursing diagnosis
Diagnosis
Anticipatory grieving related to the loss of a pregnancyOutcomes
Coping; Family coping; Grief resolutionInterventions
Grief work facilitation; Perinatal death; Active listening; PresencePlanning and implementation
Collaborative
medical.
Medical management of a tubal pregnancy depends on the patient’s condition, fetus’s gestational age and size, and whether the fallopian tube has ruptured. If the tube is intact, the gestation is less than 6 weeks, the fertilized mass is less than 3.5 cm in diameter, and the patient is hemodynamically stable with normal liver and renal function, methotrexate, a chemotherapeutic agent that inhibits cell division, may be ordered. The patient must also be committed to coming in for follow-up appointments, which are critical to maternal well-being and assessing the effectiveness of treatment. Human chorionic gonadotropin (hCG) levels and fetal cardiac activity are monitored with methotrexate therapy; success of treatment is based on these two assessments (hCG should decrease 15% by day 4, and fetal cardiac activity should cease by day 7). If the tube is damaged or ruptured, surgical management is indicated immediately.surgical.
Laparoscopic laser surgery is usually performed, but if the tube has already ruptured, a laparotomy may be indicated. A salpingectomy (removal of the tube), salpingostomy (incision and evacuation of tubal contents), salpingotomy (incision and closure of the tube), or segmental resection and anastomosis can be performed. The goal is to salvage the tube, especially in women who desire future pregnancy.Postoperative care includes monitoring vital signs and observing for other signs of shock. Monitor the fluid intake and output as well and note the color and amount of vaginal bleeding. Observe the incision for any signs and symptoms of infection. Administer analgesics and assess the patient’s level of pain relief from the medication.
Pharmacologic highlights
| Medication or Drug Class | Dosage | Description | Rationale |
|---|---|---|---|
| Methotrexate sodium (Folex) (leucovorin is also given with methotrexate if given over 4 days) | 50 mg/m2 IM or 1 mg/kg IM days 1, 3, 5, 7 | Antineoplastic, acts a folic acid antagonist | Inhibits the growth of the pregnancy by interfering with DNA, RNA, and protein synthesis |
| Analgesics | Varies by drug | Narcotics, NSAIDs; drug used depends on the level of pain | Relieve pain |
| RhoD immunoglobulin (RhoGAM) | 120–300 μg IM one time | Immune serum | Given only if mother is Rh-negative and father is Rh-positive; prevents the antigen-antibody response leading to Rh isoimmunization in future pregnancies |
Independent
Provide emotional support, using therapeutic communication techniques to relieve the patient’s anxiety. Emotional support of this patient is important because the termination of any pregnancy causes a host of psychological and physiological changes. Inform the patient of perinatal grief support groups.
The patient may be concerned about infertility. Provide information and clarify the physician’s explanations if needed. If necessary, provide a referral for a clinical nurse specialist or counselor.
Evidence-Based Practice and Health Policy
Karhus, L.L., Egerup, P., Skovlund, C.W., & Lidegaard, O. (2013). Long-term reproductive outcomes in women whose first pregnancy is ectopic: A national controlled follow-up study. Human Reproduction, 28(1), 241–246.
- Future fertility may be compromised in women who have ectopic pregnancies.
- Investigators conducted a retrospective study among a sample of 2,917 women whose first pregnancies were ectopic and compared them to a cohort of age-matched women who had first pregnancies within the same year. Findings revealed that women with ectopic pregnancies had a lower long-term rate of successful delivery (69 per 100 pregnancies) over a mean follow-up period of 23.2 years.
- Women whose first pregnancy was ectopic were 4.7 times more likely (95% CI, 3.8 to 5.8) to have future ectopic pregnancies and 45% less likely (95% CI, 0.52 to 0.58) to deliver future pregnancies successfully than the comparison cohort.
Documentation guidelines
- Physical responses: Amount and character of blood loss, vital signs, abdominal assessment (presence and description of pain, response to analgesics)
- Serial laboratory values: Hemoglobin and hematocrit, coagulation profile, white blood cell count; results of Rh test
- Response to treatments: Surgery, laparoscopy, fluid or blood replacement, medications
- Emotional status and coping abilities, partner’s response
- Presence of complications: Hemorrhage, hypovolemic shock, infection
Discharge and home healthcare guidelines
patient teaching.
If the patient is receiving methotrexate on an outpatient basis, teach her that more severe pain may indicate treatment failure and that she needs to notify the physician. She should not drink alcohol or take vitamins containing folic acid. She may experience anorexia, nausea and vomiting, mouth ulcers, and sensitivity to sunlight as side effects of methotrexate. She also needs to follow up with scheduled hCG testing.If a salpingectomy was done, explain to the patient that becoming pregnant again may be difficult. Fertilization takes place only on the side of the remaining tube after ovulation of the ovary on the same side. If a tubal repair was done, the patient is at a higher risk for a subsequent ectopic pregnancy as well as infertility. Educate the patient to recognize the signs and symptoms of ectopic pregnancy and to notify the doctor immediately if these should occur.
To prevent recurrence, advise the patient to engage in safe sexual practices. Teach her strategies to avoid STIs and pelvic infections that could cause further damage to the fallopian tubes.
postoperative instructions.
Give the patient the following instructions: Limit activity and get plenty of rest. Increase fluid intake. Keep the incision clean. Refrain from sexual intercourse for 2 weeks until the follow-up appointment with the physician occurs. Delay pregnancy for at least 3 months to allow for tubal healing. Determine that she has a method of birth control prior to leaving the hospital.referral.
If the patient is having difficulty dealing with the perinatal loss, referring her to a support group is appropriate. Often, follow-up by the hospital perinatal grief counselor is done. Referral to a fertility specialist is indicated if she is having difficulty conceiving for 6 months after tubal surgery.Patient discussion about ectopic pregnancy
Q. What is an Ectopic Pregnancy? I've heard that an ectopic pregnancy can be very dangerous. What is exactly an ectopic pregnancy?
for easier understanding, ectopic pregnancy means a pregnancy that occurs not in the normal place (uterus/womb). It talks about the implantation of the zygote (embryo).
If it is implanted in uterus wall then it is normal, if it is not in uterus wall (endometrium) then it is called ectopic pregnancy.
So ectopic pregnancy includes :
- extra-uterine pregnancy (including tuba, abdomen, ovarium)
- abnormal intra-uterine pregnancy (some doctors include : cervix, muscular wall of uterine)
Q. Do doctors normally do ultrasounds to prove you have mis carried?? 2 weeks ago i found out i was pregnant, i started spottion so we went to the hospital where they toldl me i miscarried, but they did not do any alternative tests to prove it not even check my Hcg levels. Im wandering if i should get a second opinion to make sure.
