DESCRIPTIONS OF MEDICAL FUNGI
DESCRIPTIONS OF MEDICAL FUNGI
DESCRIPTIONS OF MEDICAL FUNGI
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>DESCRIPTIONS</strong> <strong>OF</strong> <strong>MEDICAL</strong> <strong>FUNGI</strong><br />
SECOND EDITION<br />
DAVID ELLIS<br />
STEPHEN DAVIS<br />
HELEN ALEXIOU<br />
ROSEMARY HANDKE<br />
ROBYN BARTLEY<br />
MYCOLOGY UNIT<br />
WOMEN’S AND CHILDREN’S HOSPITAL<br />
SCHOOL <strong>OF</strong> MOLECULAR & BIO<strong>MEDICAL</strong> SCIENCE<br />
UNIVERSITY <strong>OF</strong> ADELAIDE<br />
ADELAIDE<br />
AUSTRALIA<br />
2007<br />
Cover: Cryptococcus neoformans, and montages including Microsporum, Candida,<br />
Schizophyllum, Sordaria, Conidiobolus, Fusarium, Bipolaris, Aspergillus, Curvularia,<br />
Saksenaea, Gliocladium, Trichophyton and Phialophora.
Published by the Authors<br />
Mycology Unit<br />
Women’s and Children’s Hospital<br />
North Adelaide 5006<br />
AUSTRALIA<br />
Direct Phone: (08) 8161 7365<br />
International + 618 8161 7365<br />
Direct Fax: (08) 8161 7589<br />
International + 618 8161 7589<br />
Email: dellis@adelaide.edu.au<br />
www.mycology.adelaide.edu.au<br />
© Copyright 2007<br />
The National Library of Australia Cataloguing-in-Publication entry:<br />
Descriptions of medical fungi.<br />
2nd ed.<br />
Bibliography.<br />
Includes index.<br />
ISBN 9780959851267 (pbk.).<br />
1. Fungi - Indexes. 2. Mycology - Indexes. I. Ellis, David (David H.).<br />
579.5<br />
Printed in Adelaide by<br />
Nexus Print Solutions<br />
153 Holbrooks Road<br />
Underdale, South Australia 2032
The Mycology Unit at the Adelaide Women’s and Children’s Hospital has played a key<br />
role in the provision of the Mycology component of the Microbiology Quality Assurance<br />
Program (QAP) organised by the Royal College of Pathologists of Australasia<br />
since its inception in 1979. The idea to provide all laboratories with a set of description<br />
sheets covering medical fungi evolved in the late 1980s and the first edition of this<br />
book was published in 1992. We now provide an updated edition which includes new<br />
and revised descriptions. We have endeavoured to reconcile current morphological<br />
descriptions with more recent genetic data, however in some cases, especially for the<br />
anthropophilic dermatophytes this is currently not possible.<br />
These descriptions have by necessity been kept brief and many have been based on<br />
previous descriptions by other authors. For further information regarding any of the<br />
mycoses or pathogenic fungi mentioned, the reader is referred to the references cited.<br />
For the precise definitions of the mycological terminology used, the reader is referred<br />
to Ainsworth and Bisby’s Dictionary of the Fungi (Kirk et al. 2001).<br />
For many species, antifungal susceptibility data has also been provided. This has<br />
been derived from both the literature and in-house data from Australian clinical isolates<br />
generated by using the CLSI M27-A2 protocol for yeasts and the CLSI M38-A protocol<br />
for moulds. This composite data is provided as a guide only. MIC 90 s for Aspergillus,<br />
Candida, Cryptococcus and Scedosporium species are provided from large Australian<br />
studies based predominantly on primary isolates. In many cases the clinical relevance<br />
of in vitro antifungal susceptibility results remains difficult to interpret, and expert advice<br />
from a consulting microbiologist or infectious disease specialist may be required.<br />
Risk group (RG) recommendations are based on published data and on current laboratory<br />
safety procedures in accordance with the Australian/New Zealand Standard AS/<br />
NZS 2243.3:2002. Safety in laboratories Part 3: Microbiological aspects and containment<br />
facilities.<br />
David Ellis BSc (Hons), MSc, PhD, FASM, FRCPA (Hon).<br />
Associate Professor<br />
School of Molecular & Biomedical Sciences<br />
University of Adelaide<br />
Head, Mycology Unit<br />
Women’s and Children’s Hospital<br />
North Adelaide, Australia 5006<br />
September, 2007<br />
PREFACE
Absidia corymbifera 1<br />
Acremonium 2<br />
Acrophialophora fusispora 3<br />
Alternaria 4<br />
Aphanoascus fulvescens 5<br />
Apophysomyces elegans 6<br />
Aspergillus 8<br />
Aspergillus flavus 9<br />
Aspergillus fumigatus 10<br />
Aspergillus nidulans 11<br />
Aspergillus niger 12<br />
Aspergillus terreus 13<br />
Aureobasidium pullulans 14<br />
Basidiobolus ranarum 15<br />
Beauveria 16<br />
Bipolaris 17<br />
Blastomyces dermatitidis 19<br />
Candida 20<br />
Candida albicans 23<br />
Candida colliculosa 24<br />
Candida dubliniensis 25<br />
Candida fabianii 26<br />
Candida famata 27<br />
Candida glabrata 28<br />
Candida guilliermondii 29<br />
Candida haemulonii 30<br />
Candida inconspicua 31<br />
Candida kefyr 32<br />
Candida krusei 33<br />
Candida lipolytica 34<br />
Candida lusitaniae 35<br />
Candida norvegensis 36<br />
Candida parapsilosis 37<br />
Candida pelliculosa 38<br />
Candida rugosa 39<br />
Candida tropicalis 40<br />
Chaetomium 41<br />
Chrysosporium tropicum 42<br />
Cladophialophora bantiana 43<br />
Cladophialophora carrionii 44<br />
Cladosporium 45<br />
Coccidioides immitis 46<br />
Colletotrichum 48<br />
Conidiobolus coronatus 49<br />
Cryptococcus 50<br />
Cryptococcus albidus 51<br />
Cryptococcus laurentii 51<br />
Cryptococcus gattii 52<br />
Cryptococcus neoformans 53<br />
CONTENTS<br />
Cunninghamella bertholletiae 55<br />
Curvularia 57<br />
Cylindrocarpon 58<br />
Drechslera 59<br />
Epicoccum purpurascens 60<br />
Epidermophyton floccosum 61<br />
Exophiala dermatitidis 62<br />
Exophiala jeanselmei complex 63<br />
Exophiala spinifera complex 65<br />
Exserohilum 66<br />
Fonsecaea 67<br />
Fusarium 68<br />
Fusarium oxysporum 69<br />
Fusarium solani 70<br />
Geotrichum candidum 71<br />
Geotrichum capitatum 72<br />
Gliocladium 73<br />
Graphium 74<br />
Histoplasma capsulatum 75<br />
Hortaea werneckii 77<br />
Lasiodiplodia theobromae 78<br />
Lecythophora hoffmannii 79<br />
Madurella grisea 80<br />
Madurella mycetomatis 81<br />
Malassezia 82<br />
Malbranchea 83<br />
Microsporum 84<br />
Microsporum audouinii 85<br />
Microsporum canis 86<br />
Microsporum canis var. distortum 88<br />
Microsporum canis var. equinum 89<br />
Microsporum cookei 90<br />
Microsporum ferrugineum 91<br />
Microsporum fulvum 92<br />
Microsporum gallinae 93<br />
Microsporum gypseum 94<br />
Microsporum nanum 95<br />
Microsporum persicolor 96<br />
Mortierella wolfii 97<br />
Mucor 98<br />
Mucor amphibiorum 99<br />
Mucor circinelloides 100<br />
Mucor indicus 100<br />
Mucor ramosissimus 100<br />
Nattrassia mangiferae 101<br />
Ochroconis gallopava 102<br />
Onychocola canadensis 103<br />
Paecilomyces 104<br />
Paecilomyces lilacinus 105
Paecilomyces variotii. 106<br />
Paracoccidioides brasiliensis 107<br />
Penicillium 108<br />
Penicillium marneffei 110<br />
Phaeoacremonium parasiticum 111<br />
Phialophora 112<br />
Phialophora richardsiae 112<br />
Phialophora verrucosa 113<br />
Phoma 114<br />
Pithomyces 115<br />
Prototheca 116<br />
Ramichloridium 117<br />
Ramichloridium schulzeri 117<br />
Rhinocladiella 118<br />
Rhinocladiella atrovirens 118<br />
Rhizomucor 119<br />
Rhizomucor miehei 119<br />
Rhizomucor pusillus 120<br />
Rhizopus 121<br />
Rhizopus azygosporus 122<br />
R. microsporus var. microsporus 122<br />
R. microsporus var. oligosporus 123<br />
R. microsporus var. rhizopodiformis 123<br />
Rhizopus oryzae 124<br />
Rhodotorula 125<br />
Rhodotorula glutinis 126<br />
Rhodotorula mucilaginosa 127<br />
Saccharomyces cerevisiae 128<br />
Saksenaea vasiformis 129<br />
Scedosporium apiospermum 131<br />
Scedosporium aurantiacum 131<br />
Scedosporium prolificans 134<br />
Schizophyllum commune 135<br />
Scopulariopsis 136<br />
Sepedonium 137<br />
Sporothrix schenckii 138<br />
Stemphylium 140<br />
Syncephalastrum 141<br />
Trichoderma 142<br />
Trichophyton 143<br />
Trichophyton ajelloi 144<br />
Trichophyton concentricum 145<br />
Trichophyton equinum 147<br />
Trichophyton erinacei 149<br />
Trichophyton interdigitale 151<br />
T. interdigitale var. nodulare 153<br />
Trichophyton mentagrophytes 154<br />
T. mentag. var. quinckeanum 156<br />
Trichophyton rubrum 158<br />
CONTENTS<br />
Trichophyton rubrum granular type 160<br />
Trichophyton schoenleinii 162<br />
Trichophyton soudanense 163<br />
Trichophyton terrestre 164<br />
Trichophyton tonsurans 165<br />
Trichophyton verrucosum 167<br />
Trichophyton violaceum 169<br />
Trichosporon 170<br />
Trichosporon asahii 171<br />
Trichosporon asteroides 172<br />
Trichosporon cutaneum 172<br />
Trichosporon inkin 172<br />
Trichosporon mucoides 173<br />
Trichosporon ovoides 173<br />
Trichothecium roseum 174<br />
Ulocladium 175<br />
Veronaea botryosa 176<br />
Verticillium 177<br />
Microscopy Stains & Techniques 178<br />
Calcofluor White with 10% KOH 178<br />
KOH with Chlorazol Black 178<br />
India Ink Mounts 178<br />
Lactophenol Cotton Blue (LPCB) 179<br />
Direct Microscopic Preparations 179<br />
Cellotape Flag Preparations 179<br />
Slide Culture Preparations 180<br />
Specialised Culture Media 181<br />
Bird seed agar 181<br />
Bromcresol Purple Milk Agar 181<br />
CDBT media 182<br />
CGB media 182<br />
Cornmeal agar 183<br />
Cornmeal glucose sucrose agar 183<br />
Czapek Dox agar 183<br />
Dixon’s agar 183<br />
Hair perforation test 184<br />
Lactritmel agar 184<br />
Littman oxgall agar 184<br />
Malt extract agar 185<br />
1% Peptone agar 185<br />
Potato dextrose agar 185<br />
Rice grain slopes 185<br />
Sabouraud dextrose agar 186<br />
Sabouraud dextrose agar 5% NaCl 186<br />
Tap water agar 187<br />
Urease agar with 0.5% glucose 187<br />
Vitamin free agar 187<br />
References 188
Descriptions of Medical Fungi<br />
Absidia corymbifera (Cohn) Saccardo & Trotter<br />
The genus Absidia is characterised by a differentiation of the hyphae into arched stolons<br />
bearing more or less verticillate sporangiophores at the raised part of the stolon<br />
(internode), and rhizoids formed at the point of contact with the substrate (at the node).<br />
This feature separates species of Absidia from the genus Rhizopus, where the sporangia<br />
arise from the nodes and are therefore found opposite the rhizoids. The sporangia<br />
are relatively small, globose, pyriform or pear-shaped and are supported by a<br />
characteristic funnel-shaped apophysis. This distinguishes Absidia from the genera<br />
Mucor and Rhizomucor, which have large, globose sporangia without an apophysis.<br />
Absidia currently contains 21 mostly soil-borne species. A. corymbifera is a known<br />
human pathogen causing pulmonary, rhinocerebral, disseminated, CNS or cutaneous<br />
zygomycosis.<br />
Colonies are fast growing, floccose, white at first becoming pale grey with age, and<br />
up to 1.5 cm high. Sporangiophores are hyaline to faintly pigmented, simple or sometimes<br />
branched, arising solitary from the stolons, in groups of three, or in whorls of up<br />
to seven. Rhizoids are very sparingly produced and may be difficult to find without the<br />
aid of a dissecting microscope to examine the colony on the agar surface. Sporangia<br />
are small (10-40 µm in diameter) and are typically pyriform in shape with a characteristic<br />
conical-shaped columella and pronounced apophysis, often with a short projection<br />
at the top. Sporangiospores vary from subglobose to oblong-ellipsoidal (3-7 x 2.5-4.5<br />
µm), hyaline to light grey and smooth-walled. Temperature: optimum 35-37 O C; maximum<br />
45 O C. RG-2 organism.<br />
For descriptions of species, keys to taxa and additional information see Ellis and Hesseltine<br />
(1965 and 1966), Hesseltine and Ellis (1964 and 1966), Nottebrock et al. (1974),<br />
O’Donnell (1979), Samson et al. (1995), Domsch et al. (1980), McGinnis (1980), de<br />
Hoog et al. (2000) and Ellis (2005b).<br />
Key Features: zygomycete, small pyriform-shaped<br />
sporangia with a characteristic conical-shaped columellae<br />
and pronounced apophysis, rapid growth at<br />
40 O C.<br />
Antifungal<br />
MIC µg/mL<br />
Range MIC90 Amphotericin B 0.03-2 1<br />
Flucytosine >256 >256<br />
Fluconazole >16 >16<br />
Itraconazole 0.03-2 0.5<br />
Posaconazole 0.03 - 1 0.25<br />
Voriconazole 2->64 >16<br />
Very limited data, antifungal susceptibility testing<br />
of individual strains is recommended. Sun et<br />
al. (2002), Dannaoui et al. (2003), Espinel-Ingroff<br />
et al. (2001), Espinel-Ingroff (2003, 2006), Singh<br />
et al. (2005), Sabatelli et al. (2006) and WCH inhouse<br />
data.<br />
15 µm<br />
1<br />
A. corymbifera showing a typical<br />
pyriform-shaped sporangium<br />
with a conical-shaped columella<br />
and pronounced apophysis (arrow).
2<br />
Descriptions of Medical Fungi<br />
Acremonium Link ex Fries<br />
Colonies are usually slow growing, often compact and moist at first, becoming powdery,<br />
suede-like or floccose with age, and may be white, grey, pink, rose or orange in<br />
colour. Hyphae are fine and hyaline and produce mostly simple awl-shaped erect phialides.<br />
Conidia are usually one-celled (ameroconidia), hyaline or pigmented, globose<br />
to cylindrical, and mostly aggregated in slimy heads at the apex of each phialide.<br />
The genus Acremonium currently contains 100 species, most are saprophytic being<br />
isolated from dead plant material and soil. However a number of species including A.<br />
falciforme, A. kiliense, A. recifei, A. alabamensis, A. roseogriseum and A. strictum are<br />
recognised as opportunistic pathogens of man and animals, causing mycetoma, mycotic<br />
keratitis and onychomycosis. RG-2 for species isolated from humans.<br />
Microconidial Fusarium isolates may be confused with Acremonium, but they usually<br />
grow faster and have colonies with a characteristic fluffy appearance.<br />
Key Features: hyphomycete with solitary, erect, hyaline, awl-shaped phialides producing<br />
single-celled, globose to cylindrical conidia, mostly in slimy heads.<br />
For descriptions of species, keys to taxa and additional information see Gams (1971),<br />
Domsch et al. (1980), Samson et al. (1995) and de Hoog et al. (2000).<br />
10 µm<br />
Acremonium showing long awl-shaped phialides producing cylindrical,<br />
one-celled conidia mostly aggregated in slimy heads at the<br />
apex of each phialide.<br />
Antifungal<br />
MIC µg/mL<br />
Range<br />
Antifungal<br />
MIC µg/mL<br />
Range<br />
Itraconazole 0.5->8 Amphotericin B 0.5-16<br />
Posaconazole 0.06-4 Caspofungin 0.03->8<br />
Voriconazole 0.06-4 Anidulafungin 0.5->8<br />
Very limited data, antifungal susceptibility testing of individual strains<br />
is recommended. Guarro et al. (1997), Pfaller et al. (1998, 2002a),<br />
Espinel-Ingroff (2003), Cuenca-Estrella et al. (2006) and WCH inhouse<br />
data.
Descriptions of Medical Fungi 3<br />
Acrophialophora fusispora (S.B. Saksena) Samson<br />
Colonies fast growing, greyish-brown with a black reverse. Conidiophores arising singly,<br />
terminally and laterally from the hyphae, erect, straight or slightly flexuose, tapering<br />
towards the apex, pale brown, rough-walled, up to 15 μm long, 2-5 μm wide, with<br />
whorls of phialides on the upper part. Phialides flask-shaped with a swollen base<br />
and a long, narrow neck, hyaline, smooth-walled or echinulate, 9-15 x 3-4.5 μm in the<br />
broadest part. Conidia in long chains, limoniform, one-celled, pale brown 5-12 x 3-6<br />
μm, smooth to finely echinulate with indistinct spiral bands. Temperature: optimum<br />
40 O C; maximum 50 O C.<br />
The genus Acrophialophora contains 3 species and is most commonly associated with<br />
soil, especially from India. A. fusispora is a rare human pathogen. RG-1 organism.<br />
Key Features: hyphomycete with flask-shaped phialides producing long chains of<br />
one-celled, limoniform, pale brown conidia, with indistinct spiral bands.<br />
For descriptions of species, keys to taxa and additional information see Domsch et al.<br />
(1980), de Hoog et al. (2000) and Al-Mohsen et al. (2000).<br />
10 μm<br />
Culture, phialides and conidia with striations (arrows) of A. fusispora.<br />
Antifungal<br />
MIC µg/mL<br />
Range<br />
Antifungal<br />
MIC µg/mL<br />
Range<br />
Fluconazole 8-32 Amphotericin B 0.25-2<br />
Itraconazole 0.06-0.125 Flucytosine >64<br />
Voriconazole 0.06 Posaconazole 0.03<br />
Very limited data, antifungal susceptibility testing of individual strains<br />
is recommended. Al-Mohsen et al. (2000) and WCH in-house data.
4<br />
Descriptions of Medical Fungi<br />
Colonies are fast growing, black to olivaceous-black or greyish, and are suede-like to<br />
floccose. Microscopically, branched acropetal chains (blastocatenate) of multicellular<br />
conidia (dictyoconidia) are produced sympodially from simple, sometimes branched,<br />
short or elongate conidiophores. Conidia are obclavate, obpyriform, sometimes ovoid<br />
or ellipsoidal, often with a short conical or cylindrical beak, pale brown, smooth-walled<br />
or verrucose.<br />
The genus contains 44 species, most are plant parasites, but a few species are ubiquitous<br />
and are also frequently soil-borne. A. alternata is the most common of these.<br />
Although usually seen as saprophytic contaminants, Alternaria species are recognised<br />
causative agents of mycotic keratitis.<br />
Alternaria species soon lose their ability to sporulate in culture. Potato dextrose agar<br />
and cornmeal agar are the most suitable media to use, and incubation under near<br />
ultra-violet light is recommended to maintain sporulation. Temperature: optimum 25-<br />
28 O C; maximum 31-32 O C. RG-1 organism.<br />
Key Features: dematiaceous hyphomycete producing chains of darkly pigmented,<br />
ovoid to obclavate dictyoconidia, often with short conical or cylindrical beaks.<br />
For descriptions of species, keys to taxa and additional information see Simmons (1967),<br />
Ellis (1971), Domsch et al. (1980), Samson et al. (1995), de Hoog et al. (2000).<br />
Antifungal<br />
Alternaria Nees ex Fries<br />
20 μm<br />
Alternaria alternata showing branched acropetal chains and multi-celled,<br />
obclavate to obpyriform conidia with short conical beaks.<br />
MIC µg/mL<br />
MIC µg/mL<br />
Range MIC90 Antifungal<br />
Range MIC90 Fluconazole 16->64 >64 Amphotericin B 0.125->16 2 (4)<br />
Itraconazole 0.125-2 1 Flucytosine >128 >128<br />
Voriconazole 0.5-2 1 Posaconazole 0.06-0.25 0.25<br />
Limited data, antifungal susceptibility testing of individual strains is recommended.<br />
McGinnis and Pasarell (1998), Pujol et al. (2000), Espinel-Ingroff et al. (2001),<br />
Espinel-Ingroff (2003), Sabatelli et al. (2006) and WCH in-house data.
Descriptions of Medical Fungi 5<br />
Aphanoascus fulvescens (Cooke) Apinis<br />
Colonies are moderately fast growing, white to tan with the production of numerous<br />
spherical, pseudoparenchymatous, buff to light brown cleistothecia (non-ostiolate<br />
ascocarps). Asci are subspherical to ellipsoidal and eight-spored. Ascospores light<br />
brown, yellowish to pale brown in mass, irregularly reticulate, lens-shaped, 3.5-4.7 x<br />
2.5-3.5 µm. Aphanoascus fulvescens has a Chrysosporium anamorph showing typical<br />
pyriform to clavate-shaped conidia with truncated bases, 15.0-17.5 x 3.7-6.0 µm,<br />
which are formed either intercalary, laterally or terminally.<br />
Aphanoascus fulvescens is a soil keratinolytic ascomycete which occasionally causes<br />
dermatomycosis in man and animals. RG-2 organism.<br />
Key Features: keratinolytic ascomycete with a Chrysosporium anamorph.<br />
For descriptions of species, keys to taxa and additional information see Domsch et al.<br />
(1980), McGinnis (1980) and de Hoog et al. (2000).<br />
100 μm<br />
10 μm<br />
Culture, cleistothecium and conidia of Aphanoascus fulvescens.
6<br />
Descriptions of Medical Fungi<br />
Apophysomyces elegans Misra, Srivastava & Lata<br />
Colonies are fast growing, white, becoming creamy white to buff with age, downy with<br />
no reverse pigment, and are composed of broad, sparsely septate (coenocytic) hyphae<br />
typical of a zygomycetous fungus. Sporangiophores are unbranched, straight or<br />
curved, slightly tapering towards the apex, up to 200 µm long, 3- 5 µm in width near<br />
the apophysis, and hyaline when young but developing a light to dark brown pigmentation<br />
and a conspicuous sub-apical thickening 10-16 µm below the apophysis with age.<br />
Sporangiophores arise at right angles from the aerial hyphae and often have a septate<br />
basal segment resembling the “foot cell” commonly seen in Aspergillus. Rhizoids are<br />
thin-walled, subhyaline and predominantly unbranched. Sporangia are multispored,<br />
small (20-50 µm diameter), typically pyriform in shape, hyaline at first, sepia-coloured<br />
when mature, columellate and strongly apophysate. Columellae are hemispherical in<br />
shape and the apophyses are distinctively funnel or bell-shaped. Sporangiospores are<br />
smooth-walled, mostly oblong, occasionally subglobose, (3-4 x 5-6 µm), subhyaline to<br />
sepia in mass. Good growth at 26 O C, 37 O C and 42 O C. RG-2 organism.<br />
Apophysomyces elegans is readily distinguishable from other zygomycetes of medical<br />
importance, especially the morphologically similar, strongly apophysate pathogen<br />
Absidia corymbifera, by having sporangiophores with distinctive funnel or bell-shaped<br />
apophyses and hemispherical-shaped columellae. In addition, there is a conspicuous<br />
pigmented sub-apical thickening which constricts the lumen of the sporangiophore<br />
below the apophysis, and there are also distinctive foot cells.<br />
Laboratory identification of this fungus may be difficult or delayed because of the<br />
mould’s failure to sporulate on the primary isolation media or on subsequent subculture<br />
onto potato dextrose agar. Sporulation may be stimulated by the use of nutrient<br />
deficient media, like cornmeal-glucose-sucrose-yeast extract agar, Czapek Dox agar,<br />
or by using the agar block method described by Ellis and Ajello (1982) and Ellis and<br />
Kaminski (1985).<br />
Key Features: zygomycete, rare human pathogen usually associated with invasive<br />
lesions following the traumatic implantation of the fungus through the skin. Soil fungus<br />
with a tropical to sub-tropical distribution. Characteristic “cocktail glass” apophysate<br />
sporangial morphology with conspicuous sub-apical thickening of the sporangiophore,<br />
rapid growth at 42 O C.<br />
For descriptions of species, keys to taxa and additional information see Cooter et al.<br />
(1990), Ellis and Ajello, (1982), Misra et al. (1979), Padhye and Ajello (1988), Lawrence<br />
et al. (1986), Wieden et al. (1985), de Hoog et al. (2000) and Ellis (2005b).<br />
Antifungal<br />
MIC µg/mL<br />
MIC µg/mL<br />
Antifungal<br />
Range Range<br />
Fluconazole >64 Amphotericin B 0.03-2<br />
Itraconazole 0.03-8 Flucytosine >256<br />
Posaconazole 0.03-4 Voriconazole 8->64<br />
Very limited data, antifungal susceptibility testing of individual strains is<br />
recommended. Sun et al. (2002), Dannaoui et al. (2003), Sabatelli et al.<br />
(2006) and WCH in-house data.
Descriptions of Medical Fungi 7<br />
Apophysomyces elegans Misra, Srivastava & Lata<br />
10 μm 10 μm<br />
a b<br />
(a) Young, multispored, pyriform sporangium of A. elegans showing a typical funnel-shaped<br />
apophysis but without the sub-apical thickening of a more mature<br />
sporangiophore. (b) Mature sporangium of A. elegans showing distinctive funnel-shaped<br />
apophyses, columellae, and a conspicuous pigmented sub-apical<br />
thickening which constricts the lumen of the sporangiophore below the apophysis<br />
(arrow). Sporangiospores are smooth-walled, oblong and subhyaline.
8<br />
Descriptions of Medical Fungi<br />
Aspergillus Micheli ex Link<br />
Colonies are usually fast growing, white, yellow, yellow-brown, brown to black or<br />
shades of green, mostly consisting of a dense felt of erect conidiophores. Conidiophores<br />
terminate in a vesicle covered with either a single palisade-like layer of phialides<br />
(uniseriate) or a layer of subtending cells (metulae) which bear small whorls of<br />
phialides (the so called biseriate structure). The vesicle, phialides, metulae (if present)<br />
and conidia form the conidial head. Conidia are one-celled, smooth or rough walled,<br />
hyaline or pigmented are produced in long dry chains which may be divergent (radiate)<br />
or aggregated in compact columns (columnar). Some species may produce Hülle cells<br />
or sclerotia.<br />
For identification, isolates are usually inoculated at three points on Czapek Dox agar<br />
and 2% malt extract agar and incubated at 25 O C. Most species sporulate within 7<br />
days. Descriptions are primarily based on colony pigmentation and morphology of the<br />
conidial head. Microscopic mounts are best made using cellotape flag or slide culture<br />
preparations mounted in lactophenol cotton blue. A drop of alcohol is usually needed<br />
to remove bubbles and excess conidia.<br />
Key Features: hyaline hyphomycete showing distinctive conidial heads with flaskshaped<br />
phialides arranged in whorls on a vesicle.<br />
For descriptions of species, keys to taxa and additional information see Raper and<br />
Fennell (1965), Domsch et al. (1980), McGinnis (1980), Onions et al. (1981), Samson<br />
and Pitt (1990), Samson et al. (1995), de Hoog et al. (2000) and Klich (2002).<br />
a<br />
conidia<br />
phialides<br />
vesicle<br />
stipe<br />
metulae<br />
Conidial head morphology in Aspergillus (a) uniseriate, (b) biseriate.<br />
b
Descriptions of Medical Fungi 9<br />
On Czapek Dox agar, colonies are granular,<br />
flat, often with radial grooves, yellow<br />
at first but quickly becoming bright to dark<br />
yellow-green with age. Conidial heads<br />
are typically radiate, later splitting to form<br />
loose columns (mostly 300-400 µm in diameter),<br />
biseriate but having some heads<br />
with phialides borne directly on the vesicle<br />
(uniseriate). Conidiophore stipes are<br />
hyaline and coarsely roughened, often<br />
more noticeable near the vesicle. Conidia<br />
are globose to subglobose (3-6 µm in<br />
diameter), pale green and conspicuously<br />
echinulate. Some strains produce brownish<br />
sclerotia.<br />
A. flavus has a world-wide distribution and<br />
normally occurs as a saprophyte in soil<br />
and on many kinds of decaying organic<br />
matter, however, it is also a recognised<br />
pathogen of humans and animals. RG-2<br />
organism.<br />
Key Features: spreading yellow-green<br />
colonies, rough-walled stipes, mature<br />
vesicles bearing phialides over their entire<br />
surface and conspicuously echinulate<br />
conidia.<br />
Antifungal<br />
MIC µg/mL<br />
Range MIC90 Amphotericin B 0.06->8 4<br />
Itraconazole 0.03-8 0.5<br />
Voriconazole 0.03-2 0.5<br />
Posaconazole 0.03-1 0.5<br />
Anidulafungin
10<br />
Descriptions of Medical Fungi<br />
On Czapek Dox agar, colonies show typical<br />
blue-green surface pigmentation with<br />
a suede-like surface consisting of a dense<br />
felt of conidiophores. Conidial heads are<br />
typically columnar (up to 400 x 50 µm<br />
but often much shorter and smaller) and<br />
uniseriate. Conidiophore stipes are short,<br />
smooth-walled and have conical-shaped<br />
terminal vesicles which support a single<br />
row of phialides on the upper two thirds<br />
of the vesicle. Conidia are produced in<br />
basipetal succession forming long chains<br />
and are globose to subglobose (2.5-3.0<br />
µm in diameter), green and rough-walled<br />
to echinulate. Note: This species is thermotolerant<br />
and grows at temperatures up<br />
to 55 O C.<br />
A. fumigatus is truly a cosmopolitan mould<br />
and has been found almost everywhere<br />
on every conceivable type of substrate. It<br />
is an important pathogen of humans and<br />
animals. RG-2 organism.<br />
Key Features: uniseriate and columnar<br />
conidial heads with the phialides limited<br />
to the upper two thirds of the vesicle and<br />
curving to be roughly parallel to each<br />
other.<br />
Antifungal<br />
MIC µg/mL<br />
Range MIC90 Amphotericin B 0.03->8 2<br />
Itraconazole 16 0.5<br />
Voriconazole
Descriptions of Medical Fungi 11<br />
Aspergillus nidulans (Eidam) Wint.<br />
Teleomorph: Emericella nidulans (Eidam) Vuill.<br />
On Czapek Dox agar, colonies are typically plain green in colour with dark red-brown<br />
cleistothecia developing within and upon the conidial layer. Reverse may be olive to<br />
drab-grey or purple-brown. Conidial heads are short columnar (up to 70 x 30 µm in<br />
diameter) and biseriate. Conidiophore stipes are usually short, brownish and smoothwalled.<br />
Conidia are globose (3-3.5 µm in diameter) and rough-walled.<br />
A. nidulans is a typical soil fungus with a world-wide distribution, it has also been reported<br />
causing disease in human and animals. RG-1 organism.<br />
Key Features: conidial heads are short columnar and biseriate. Stipes are usually<br />
short, brownish and smooth-walled. Conidia are globose and rough-walled.<br />
20 μm<br />
10 μm 20 μm<br />
a b c<br />
(a) Cleistothecium of Emericella nidulans (anamorph Aspergillus nidulans) showing<br />
numerous reddish-brown ascospores and thick-walled hülle cells; (b) cleistothecia are<br />
often surrounded by a mass of hülle cells which are up to 25 µm in diameter; (c) conidial<br />
head and stipe and (d) culture of A. nidulans.<br />
Antifungal<br />
MIC µg/mL<br />
Range MIC90 Amphotericin B 0.125-4 2<br />
Itraconazole 0.03-8 0.25<br />
Voriconazole 0.125-4 0.25<br />
Posaconazole 0.03-1 0.25<br />
Caspofungin 0.125-8 nd<br />
Espinel-Ingroff et al. (2001), Espinel-Ingroff<br />
(2003), Cuenca-Estrella et al. (2006).<br />
MIC s from Australian clinical isolates (nd<br />
90<br />
= not done).<br />
d
12<br />
Descriptions of Medical Fungi<br />
On Czapek Dox agar, colonies consist of<br />
a compact white or yellow basal felt covered<br />
by a dense layer of dark-brown to<br />
black conidial heads. Conidial heads are<br />
large (up to 3 mm by 15 to 20 µm in diameter),<br />
globose, dark brown, becoming<br />
radiate and tending to split into several<br />
loose columns with age. Conidiophore<br />
stipes are smooth-walled, hyaline or turning<br />
dark towards the vesicle. Conidial<br />
heads are biseriate with the phialides<br />
borne on brown, often septate metulae.<br />
Conidia are globose to subglobose (3.5-5<br />
µm in diameter), dark brown to black and<br />
rough-walled.<br />
A. niger is one of the most common and<br />
easily identifiable species of the genus<br />
Aspergillus, with its white to yellow mat<br />
later bearing black conidia. This species<br />
is very commonly found in aspergillomas<br />
and is the most frequently encountered<br />
agent of otomycosis. It is also a common<br />
laboratory contaminant. RG-1 organism.<br />
Key Features: conidial heads are dark<br />
brown to black, radiate and biseriate with<br />
metulae twice as long as the phialides.<br />
Conidia brown and rough-walled.<br />
Antifungal<br />
MIC µg/mL<br />
Range MIC90 Amphotericin B 0.125-2 2<br />
Itraconazole 0.03->8 0.5<br />
Voriconazole
Descriptions of Medical Fungi 13<br />
On Czapek Dox agar, colonies are typically<br />
suede-like and cinnamon-buff to<br />
sand brown in colour with a yellow to deep<br />
dirty brown reverse. Conidial heads are<br />
compact, columnar (up to 500 x 30-50 µm<br />
in diameter) and biseriate. Conidiophore<br />
stipes are hyaline and smooth-walled.<br />
Conidia are globose to ellipsoidal (1.5-2.5<br />
µm in diameter), hyaline to slightly yellow<br />
and smooth-walled.<br />
A. terreus occurs commonly in soil and is<br />
occasionally reported as a pathogen of<br />
humans and animals. RG-2 organism.<br />
Key Features: cinnamon-brown cultures,<br />
conidial heads biseriate with metulae as<br />
long as the phialides.<br />
For descriptions of species, keys to taxa<br />
and additional information see Raper and<br />
Fennell (1965), Domsch et al. (1980),<br />
McGinnis (1980), Onions et al. (1981),<br />
Samson and Pitt (1990), Samson et al.<br />
(1995), de Hoog et al. (2000) and Klich<br />
(2002).<br />
Antifungal<br />
MIC µg/mL<br />
Range MIC90 Amphotericin B 0.06-16 4<br />
Itraconazole 0.03-1 0.25<br />
Voriconazole 0.06-2 0.25<br />
Posaconazole 0.03-2 0.125<br />
Anidulafungin 0.03 nd<br />
Caspofungin 0.015-0.5 nd<br />
Espinel-Ingroff et al. (2001), Pfaller et<br />
al. (2002), Diekema et al. (2003), Espinel-Ingroff<br />
(2003), Serrano et al. (2003),<br />
Cuenca-Estrella et al. (2006). MIC s 90<br />
from Australian clinical isolates (nd = not<br />
done).<br />
Aspergillus terreus Thom<br />
10 μm<br />
Culture and conidial head and conidiophore<br />
of A. terreus. Note: conidial heads<br />
are biseriate.
14<br />
Descriptions of Medical Fungi<br />
Aureobasidium pullulans (de Bary) Arnaud<br />
Colonies are fast growing, smooth, soon covered with slimy masses of conidia, cream<br />
or pink to brown or black. Hyphae hyaline and septate, frequently becoming darkbrown<br />
with age and forming chains of one- to two-celled, thick-walled, darkly pigmented<br />
arthroconidia. These arthroconidia actually represent the Scytalidium anamorph of<br />
Aureobasidium and are only of secondary importance in recognising members of this<br />
genus. Conidia are produced synchronously in dense groups from indistinct scars or<br />
from short denticles on undifferentiated, hyaline to sub-hyaline hyphae. Conidia are<br />
hyaline, smooth-walled, single-celled, ellipsoidal but of very variable shape and size<br />
(8-12 x 4-6 µm), often with an indistinct hilum (= a mark or scar at the point of attachment).<br />
Temperature: optimum 25 O C; maximum 35-37 O C.<br />
This species has two varieties: A. pullulans var. pullulans, with a colony which remains<br />
pink, light brown, or yellow for at least three weeks, and A. pullulans var. melanogenum<br />
which soon becomes black or greenish-black due to dark hyphae which often fall apart<br />
into separate cells. A. pullulans has a world-wide distribution and is usually isolated<br />
as a saprophyte, occasionally from skin and nails. However, it has also been reported<br />
as a rare causative agent of phaeohyphomycosis, mycotic keratitis and peritonitis in<br />
patients on continuous ambulatory peritoneal dialysis (CAPD). RG-1 organism.<br />
Key Features: hyphomycete (so called black yeast) producing hyaline blastoconidia<br />
simultaneously from the vegetative hyphae, which may also form chains of darkly pigmented,<br />
thick-walled arthroconidia.<br />
For descriptions of species, keys to taxa and additional information see Hermanides-<br />
Nijhof (1977), Domsch et al. (1980), McGinnis (1980) and de Hoog et al. 2000.<br />
20 μm<br />
A. pullulans showing chains of one- to two-celled, darkly pigmented arthroconidia of<br />
the Scytalidium anamorph of Aureobasidium and the presence of numerous hyaline,<br />
single-celled, ovoid-shaped conidia which are produced on short denticles.<br />
Antifungal<br />
MIC µg/mL MIC µg/mL MIC µg/mL<br />
Antifungal Antifungal<br />
Range Range Range<br />
Amphotericin B 0.125-2 Itraconazole 0.03-0.25 Voriconazole 0.03-0.5<br />
Very limited data, antifungal susceptibility testing of individual strains is recommended.<br />
McGinnis and Pasarell (1998), Espinel-Ingroff et al. (2001) and WCH in-house data.
Descriptions of Medical Fungi 15<br />
Synonyms: Basidiobolus meristosporus Drechsler; Basidiobolus heterosporus Srinivasan<br />
& Thirumalachar; Basidiobolus haptosporus Drechsler.<br />
Colonies are moderately fast growing at 30 O C, flat, yellowish-grey to creamy-grey, glabrous,<br />
becoming radially folded and covered by a fine, powdery, white surface mycelium.<br />
Note: satellite colonies are often formed by germinating conidia ejected from<br />
the primary colony. Microscopic examination usually shows the presence of large<br />
vegetative hyphae (8-20 µm in diameter) forming numerous round (20-50 µm in diameter),<br />
smooth, thick-walled zygospores that have two closely appressed beak-like<br />
appendages. The production of “beaked” zygospores is diagnostic for the genus. Two<br />
types of asexual conidia are formed, although isolates often lose their sporulating ability<br />
with subculture and special media incorporating glucosamine hydrochloride and<br />
casein hydrolsate may be needed to stimulate sporulation (Shipton and Zahari, 1987).<br />
Primary conidia are globose, one-celled, solitary and are forcibly discharged from a<br />
sporophore. The sporophore has a distinct swollen area just below the conidium that<br />
actively participates in the discharge of the conidium. Secondary (replicative) conidia<br />
are clavate, one-celled and are passively released from a sporophore. These sporophores<br />
are not swollen at their bases. The apex of the passively released spore has<br />
a knob-like adhesive tip. These spores may function as sporangia, producing several<br />
sporangiospores. RG-2 organism.<br />
Basidiobolus ranarum is commonly present in decaying fruit and vegetable matter, and<br />
as a commensal in the intestinal tract of frogs, toads and lizards. It has been reported<br />
from tropical Africa, India, Indonesia and South East Asia including Australia.<br />
For descriptions of species, keys to taxa and additional information see Strinivasan and<br />
Thirumalachar (1965), Greer and Friedman (1966), Dworzack et al. (1978), McGinnis<br />
(1980), King (1983), Rippon (1988), Davis et al. (1994), Jong and Dugan (2003), de<br />
Hoog et al. (2000) and Ellis (2005a).<br />
20 μm<br />
Basidiobolus ranarum Eidem<br />
a 20 μm<br />
b<br />
(a) Sporophore and conidia and (b) zygospores of Basidiobolus ranarum.
16<br />
Descriptions of Medical Fungi<br />
Colonies are usually slow growing, mostly not exceeding 2 cm in ten days at 20 O C,<br />
downy, at first white but later often becoming yellow to pinkish. The genus Beauveria<br />
is characterised by the sympodial development of single-celled conidia (ameroconidia)<br />
on a geniculate or zig-zag rachis. Conidiogenous cells are flask-shaped, rachiform,<br />
proliferating sympodially and are often aggregated into sporodochia or synnemata.<br />
Conidia are hyaline and globose or ovoid in shape. RG-1 organism.<br />
Three species are recognised, two of which are well known parasites of insects. B.<br />
bassiana is the most common species and is best known as the causal agent of the<br />
disastrous muscardine in silkworms. Beauveria species are occasionally isolated in<br />
the clinical laboratory as saprophytic contaminants.<br />
Key Features: hyphomycete showing sympodial development of ameroconidia on a<br />
geniculate or zig-zag rachis emanating from a flask-shaped conidiophore.<br />
For descriptions of species, keys to taxa and additional information see de Hoog (1972),<br />
Domsch et al. (1980), McGinnis (1980) and de Hoog et al. (2000).<br />
20 μm<br />
Beauveria Vuillemin<br />
Beauveria bassiana showing sympodial development of conidia on a geniculate<br />
or zig-zag rachis. Conidiogenous cells are flask-shaped, rachiform,<br />
proliferating sympodially and are often aggregated into sporodochia or synnemata.<br />
Conidia are hyaline and globose or ovoid in shape, 2-3 mm diameter<br />
(phase contrast image).
Descriptions of Medical Fungi 17<br />
Teleomorph: Cochliobolus Drechsler<br />
Bipolaris Shoemaker<br />
Colonies are moderately fast growing, effuse, grey to blackish brown, suede-like to<br />
floccose with a black reverse. Microscopic morphology shows sympodial development<br />
of pale brown pigmented, pseudoseptate conidia on a geniculate or zig-zag rachis.<br />
Conidia are produced through pores in the conidiophore wall (poroconidia) and are<br />
straight, fusiform to ellipsoidal, rounded at both ends, smooth to finely roughened, germinating<br />
only from the ends (bipolar).<br />
The genus Bipolaris contains about 45 species which are mostly subtropical and tropical<br />
plant parasites; however several species, notably B. australiensis, B. hawaiiensis<br />
and B. spicifera are well documented human pathogens. RG-1 organisms.<br />
Key Features: dematiaceous hyphomycete producing sympodial, pseudoseptate, pale<br />
brown, straight, fusiform to ellipsoidal poroconidia, which are rounded at both ends.<br />
The genera Drechslera, Bipolaris, Curvularia and Exserohilum are all closely related<br />
and differentiation of the genera relies upon a combination of characters including conidial<br />
shape, the presence or absence of a protruding hilum, the contour of the basal<br />
portion of the conidium and its hilum, the point at which the germ tube originates from<br />
the basal cell and, to a lesser degree, the sequence and location of the first three conidial<br />
septa. The table below is modified from Domsch et al. (1980).<br />
Anamorph Main characters Teleomorph<br />
Drechslera Conidia cylindrical, germinating from any cell,<br />
hilum not protuberant<br />
Bipolaris Conidia fusiform-ellipsoidal, central cells not<br />
much darker and broader than the distal ones,<br />
hilum not protuberant, germination bipolar.<br />
Curvularia Conidia with 2-3 broader and darker central<br />
cells, often curved, with or without a prominent<br />
hilum, germination bipolar.<br />
Exserohilum Conidia fusiform-cylindrical to obclavate, with<br />
a protuberant hilum germination bipolar.<br />
Pyrenophora<br />
Cochliobolus<br />
Cochliobolus<br />
Setosphaeria<br />
Species of Bipolaris, Curvularia and Exserohilum are causative agents of phaeohyphomycosis<br />
which is an emerging mycotic infection of humans and lower animals<br />
caused by a number of dematiaceous (brown-pigmented) fungi where the tissue morphology<br />
of the causative organism is mycelial. This separates it from other clinical<br />
types of disease involving brown-pigmented fungi where the tissue morphology of the<br />
organism is a grain (mycotic mycetoma) or sclerotic body (chromoblastomycosis).<br />
For descriptions of species, keys to taxa and additional information see Ellis (1971<br />
and 1976), Luttrell (1978), Domsch et al. (1980), Alcorn (1983), Padhye et al. (1986),<br />
McGinnis et al. (1986b), Sivanesan (1987), Rippon (1988) and de Hoog et al. (2000).<br />
Also see Descriptions for Curvularia, Drechslera and Exserohilum.
18<br />
Descriptions of Medical Fungi<br />
10 μm<br />
Bipolaris australiensis showing sympodial development of pale<br />
brown, fusiform to ellipsoidal, pseudoseptate, poroconidia on a<br />
geniculate or zig-zag rachis.<br />
Antifungal<br />
Bipolaris Shoemaker<br />
MIC µg/mL<br />
MIC µg/mL<br />
Range<br />
Antifungal<br />
Range<br />
Itraconazole 0.03-1 Amphotericin B 0.06-2<br />
Posaconazole 0.06-0.05 Anidulafungin 1-4<br />
Voriconazole 0.06-0.05 Caspofungin 1-4<br />
Limited data, antifungal susceptibility testing of individual strains is recommended.<br />
Espinel-Ingroff et al. (2001), Pfaller et al. (2002a), Espinel-Ingroff<br />
(2003), McGinnis and Pasarell (1998) and WCH in-house data.
Descriptions of Medical Fungi 19<br />
Blastomyces dermatitidis Gilchrist & Stokes<br />
Colonies (SDA) at 25 O C are variable in morphology and rate of growth. They may grow<br />
rapidly, producing a fluffy white mycelium or slowly as glabrous, tan, nonsporulating<br />
colonies (Fig. a). Growth and sporulation may be enhanced by yeast extract. Most<br />
strains become pleomorphic with age. Microscopically, hyaline, ovoid to pyriform, onecelled,<br />
smooth-walled conidia (2-10 µm in diameter) of the Chrysosporium type, are<br />
borne on short lateral or terminal hyphal branches.<br />
Colonies on blood agar at 37 O C are wrinkled and folded, glabrous and yeast-like. Microscopically,<br />
the organism produces the characteristic yeast phase as seen in tissue<br />
pathology; ie. B. dermatitidis is a dimorphic fungus.<br />
WARNING: RG-3 organism. Cultures of Blastomyces dermatitidis may represent a<br />
biohazard to laboratory personnel and should be handled in an appropriate pathogen<br />
handling cabinet. In the past, conversion from the mould form to the yeast form was<br />
necessary to positively identify this dimorphic pathogen from species of Chrysosporium<br />
or Sepedonium; however, culture identification by exoantigen test is now the method<br />
of choice.<br />
Histopathology: Tissue sections show large, broad-based, unipolar budding yeastlike<br />
cells, which may vary in size from 8-15 µm (Fig. b), with some larger forms up to<br />
30 µm in diameter. Note: tissue sections need to be stained by Grocott’s methenamine<br />
silver method to clearly see the yeast-like cells, which are often difficult to observe in<br />
H&E preparations.<br />
Key Features: clinical history, tissue pathology, culture identification by positive<br />
exoantigen test.<br />
For descriptions of species, keys to taxa and additional information see McGinnis<br />
(1980), Chandler et al. (1980), Kaufman and Standard (1987) and Rippon (1988).<br />
Antifungal<br />
a b<br />
10 μm<br />
MIC µg/mL<br />
MIC µg/mL<br />
Antifungal<br />
Range MIC Range MIC 90 90<br />
Fluconazole 0.125-64 4-16 Amphotericin B 0.03-1 0.5<br />
Itraconazole 0.03->16 0.125-2 Voriconazole 0.03-16 0.25<br />
Posaconazole 0.03-2 0.125 Caspofungin 0.5-8 2<br />
Limited data available. Sugar and Liu (1996), Espinel-Ingroff et al. (2001),<br />
Espinel-Ingroff (2003), Gonzales et al. (2005) and Sabatelli et al. (2006).
20<br />
Descriptions of Medical Fungi<br />
The genus Candida is characterised by globose to elongate yeast-like cells or blastoconidia<br />
that reproduce by multilateral budding, polar budding if present on a narrow<br />
base, pseudohyphae and occasionally true hyphae may also be present. Arthroconidia,<br />
ballistoconidia and colony pigmentation are always absent. Fermentation or<br />
not: Nitrate assimilation or not: Inositol assimilation or not, however all inositol positive<br />
strains form pseudohyphae. In the past, the genus Torulopsis was separated from<br />
the genus Candida by the absence of pseudomycelium. However, in 1978 Yarrow &<br />
Meyer amended the description of Candida to include all species previously included<br />
in Torulopsis.<br />
Several species of Candida may be aetiological agents, most commonly C. albicans,<br />
followed by C. parapsilosis, C. glabrata, C. krusei and C. tropicalis. However a number<br />
of other species may also be isolated (see table below). All are ubiquitous and occur<br />
naturally on humans.<br />
Identification:<br />
Candida Berkhout<br />
Ensure that you start with a fresh growing pure culture; streak for single colony isolation<br />
if necessary.<br />
Chromogenic agars are now being used for primary isolation for both the detection of<br />
mixed flora and rapid species identification, especially from non-sterile sites.<br />
Germ Tube Test. A rapid screening test for Candida albicans and Candida dubliniensis.<br />
0.5 mL of serum, containing 0.5% glucose, is lightly inoculated with the test organism<br />
and incubated at 35 O C for 2-3 hours. On microscopy, the production of germ tubes by<br />
the cells is diagnostic for Candida albicans.<br />
10 μm<br />
Production of germ tubes by C. albicans.<br />
Species distribution from 944 patients<br />
with candidemia (Australian<br />
Candidemia Study 2002-2004).<br />
Species No %<br />
C. albicans 447 47.3<br />
C. parapsilosis 182 19.3<br />
C. glabrata 167 17.8<br />
C. krusei 46 4.9<br />
C. tropicalis 46 4.9<br />
C. dubliniensis 22 2.3<br />
C. guilliermondii 11 1.2<br />
C. lusitaniae 8 0.8<br />
C. kefyr 5 0.5<br />
C. pelliculosa 3 0.3<br />
C. rugosa 2 0.2<br />
C. colliculosa 1 0.1<br />
C. famata 1 0.1<br />
C. inconspicua 1 0.1<br />
C. lipolytica 1 0.1<br />
C. fabianii 1 0.1
Descriptions of Medical Fungi 21<br />
Candida Berkhout<br />
For the full identification of germ tube negative yeasts, morphological (Dalmau<br />
plate culture), physiological and biochemical tests are essential.<br />
(a) Dalmau Plate Culture: To set up a yeast morphology plate, dip a flamed sterilised<br />
straight wire into a culture to make a light inoculum and then lightly scratch the wire<br />
into the surface of a cornmeal/tween 80, rice/tween 80 or yeast morphology agar plate,<br />
then place a flamed coverslip onto the agar surface covering the scratches. Dalmau<br />
morphology plates are examined in-situ directly under the lower power of a microscope<br />
for the presence of pseudohyphae which may take up to 4-5 days at 26 O C to develop.<br />
Candida albicans also produces characteristic large, round, terminal, thick-walled vesicles<br />
(often called chlamydospores). The key features to remember are to use a light<br />
inoculum and to scratch the surface of the agar with the wire when inoculating.<br />
(b) Physiological and biochemical tests including fermentation and assimilation studies<br />
should be performed based on those used at the Centraalbureau voor Schimmelcultures,<br />
Utrecht, The Netherlands. Reference “The Yeasts: a taxonomic study”, edited<br />
by Kurtzman and Fell (1998), Elsevier Science Publishers B.V. Amsterdam. Reliable<br />
commercially available yeast identification kits are the API 20C, ID32C, MicroScan and<br />
Vitek systems. For specific identification of species see appropriate text book.<br />
5 mm 10 μm<br />
a b<br />
(a) Dalmau plate culture showing colonies of C. albicans growing out from scratches<br />
on the surface of a cornmeal/tween 80 agar plate. Note: a coverslip has been placed<br />
onto the agar surface covering the scratches. (b) Confirmatory test for C. albicans.<br />
Production of large round, thick-walled vesicles (often called chlamydospores) in<br />
Dalmau plate cultures.<br />
For descriptions of species, keys to taxa and additional information see Barnett et al.<br />
(1983), Kurtzman and Fell (1988) and de Hoog et al. (2000).
22<br />
Descriptions of Medical Fungi<br />
Candida albicans (Robin) Berkhout<br />
10 μm<br />
10 μm<br />
CHROMagar Candida plate<br />
showing chromogenic colour<br />
change for C. albicans (green),<br />
C. tropicalis (blue), C. parapsilosis<br />
(white) and C. glabrata<br />
(pink).<br />
Candida albicans on Sabouraud’s<br />
dextrose agar showing<br />
typical cream coloured, smooth<br />
surfaced, waxy colonies.<br />
Direct smear of urine from a<br />
patient with candidiasis of the<br />
kidney showing C. albicans in<br />
mycelial or tissue phase with<br />
blastoconidia budding from the<br />
pseudohyphae.<br />
Microscopic morphology of<br />
C. albicans showing budding<br />
spherical to ovoid blastoconidia.
Descriptions of Medical Fungi 23<br />
Candida albicans (Robin) Berkhout<br />
Culture: Colonies (SDA) white to cream-coloured smooth, glabrous yeast-like.<br />
Microscopy: Spherical to subspherical budding blastoconidia, 2-7 x 3-8 µm in size.<br />
India Ink Preparation: Negative - No capsules present.<br />
Dalmau Plate Culture on Cornmeal and Tween 80 Agar: Branched pseudohyphae<br />
with dense verticils of blastoconidia. Spherical chlamydospores, mostly terminal, often<br />
on a slightly swollen subtending cell are formed near the edge of the cover slip.<br />
Physiological Tests: + Positive, - Negative, v Variable, w Weak, s Slow<br />
Germ Tube + L-Sorbose v L-Arabinose v D-Glucitol -(s)<br />
Fermentation Sucrose v D-Arabinose v α-M-D-glucoside v<br />
Glucose + Maltose + D-Ribose -(s) D-Gluconate -(s)<br />
Galactose v Cellobiose - L-Rhamnose - DL-Lactate +<br />
Sucrose -(s) Trehalose +(s) D-Glucosamine v myo-Inositol +<br />
Maltose + Lactose - N-A-D-glucosamine + 2-K-D-gluconate +<br />
Lactose - Melibiose - Glycerol v D-Glucuronate -<br />
Trehalose v Raffinose - Erythritol - Nitrate -<br />
Assimilation Melezitose v Ribitol v Urease -<br />
Glucose + Soluble Starch + Galactitol - 0.1% Cycloheximide +<br />
Galactose + D-Xylose + D-Mannitol + Growth at 40 O C +<br />
Key Features: germ tube positive, production of chlamydospores on Dalmau plate<br />
culture, fermentation of glucose, sugar assimilation profile and a distinctive green<br />
colour on CHROMagar. Note: germ tube negative variants, known as C. claussenii,<br />
and sucrose-negative variants described as C. stellatoidea have proven to be<br />
synonymous with C. albicans. C. albicans is a commensal of mucous membranes<br />
and the gastrointestinal tract. Environmental isolations have been made from sources<br />
contaminated by human or animal excreta, such as polluted water, soil, air and plants.<br />
RG-2 organism.<br />
Antifungal<br />
MIC µg/mL<br />
MIC µg/mL<br />
Antifungal<br />
Range MIC Range MIC 90 90<br />
Fluconazole 0.03->64 2 Amphotericin B 0.03-4 0.25<br />
Itraconazole 0.008->8 0.125 Flucytosine 0.03->64 0.5<br />
Posaconazole 0.008->8 0.016 Caspofungin 0.008->4 0.125<br />
Voriconazole 0.008->8 0.03 Anidulafungin 0.008->8 nd<br />
Good data available. Espinel-Ingroff et al. (2001), Pfaller et al. (2002b, 2006, 2007),<br />
Espinel-Ingroff (2003), Hajjeh et al. (2004), Richter et al. (2005) and Cuenca-Estrella<br />
et al. (2006). MIC 90 s from the Australian Candidemia Study (nd = not done).
24<br />
Descriptions of Medical Fungi<br />
Candida colliculosa (Hartmann) S.A. Meyer & Yarrow<br />
Teleomorph: Torulaspora delbrueckii (Lindner) Lindner.<br />
Culture: Colonies (SDA) white to cream-coloured smooth, glabrous yeast-like.<br />
Microscopy: Spherical to ellipsoidal budding blastoconidia, 2-6 x 3-7 µm in size. Ascospores<br />
may be produced on 5% malt extract or cornmeal agar after 5-30 days at<br />
25 O C.<br />
India Ink Preparation: Negative - No capsules present.<br />
Dalmau Plate Culture on Cornmeal and Tween 80 Agar: Budding yeast cells only.<br />
No pseudohyphae or true hyphae produced.<br />
Physiological Tests: + Positive, - Negative, v Variable, w Weak, s Slow<br />
Germ Tube - L-Sorbose v L-Arabinose - D-Glucitol v<br />
Fermentation Sucrose v D-Arabinose - α-M-D-glucoside v<br />
Glucose + Maltose v D-Ribose - D-Gluconate v<br />
Galactose v Cellobiose - L-Rhamnose - DL-Lactate v<br />
Sucrose v Trehalose -,s D-Glucosamine - myo-Inositol -<br />
Maltose v Lactose - N-A-D-glucosamine - 2-K-D-gluconate +<br />
Lactose - Melibiose - Glycerol v D-Glucuronate v<br />
Trehalose v Raffinose v Erythritol - Nitrate -<br />
Assimilation Melezitose v Ribitol v Urease -<br />
Glucose + Soluble Starch - Galactitol - 0.1% Cycloheximide -<br />
Galactose v D-Xylose v D-Mannitol + Growth at 37 O C v<br />
Key Features: asci containing 1-4 spheroidal ascospores, variable growth at 37 O C<br />
and a variable sugar assimilation profile. C. colliculosa is a rare cause of candidemia.<br />
RG-1 organism.<br />
Antifungal<br />
MIC µg/mL<br />
MIC µg/mL<br />
Range Antifungal<br />
Range<br />
Fluconazole 8 Amphotericin B 0.25<br />
Itraconazole 0.25 Flucytosine 0.03<br />
Posaconazole 0.25 Caspofungin 0.06<br />
Voriconazole 0.06 Anidulafungin nd<br />
Very limited data, antifungal susceptibility testing of individual stains is recommended.<br />
Data from the Australian Candidemia Study (nd = not done).
Descriptions of Medical Fungi 25<br />
Candida dubliniensis Sullivan et al.<br />
Culture: Colonies (SDA) white to cream-coloured smooth, glabrous yeast-like.<br />
Microscopy: Spherical to subspherical budding blastoconidia, 3-8 x 2-7 µm in size.<br />
India Ink Preparation: Negative - No capsules present.<br />
Dalmau Plate Culture on Cornmeal and Tween 80 Agar: Branched pseudohyphae<br />
with dense verticils of blastoconidia and spherical, mostly terminal chlamydospores.<br />
Physiological Tests: + Positive, - Negative, v Variable, w Weak, s Slow<br />
Germ Tube + L-Sorbose - L-Arabinose - D-Glucitol +<br />
Fermentation Sucrose + D-Arabinose - α-M-D-glucoside +,s<br />
Glucose + Maltose + D-Ribose - D-Gluconate -,s<br />
Galactose v Cellobiose - L-Rhamnose - DL-Lactate +<br />
Sucrose - Trehalose + D-Glucosamine -,s myo-Inositol -<br />
Maltose + Lactose - N-A-D-glucosamine + 2-K-D-gluconate +<br />
Lactose - Melibiose v Glycerol +,s D-Glucuronate -<br />
Trehalose v Raffinose - Erythritol - Nitrate -<br />
Assimilation Melezitose + Ribitol +,s Urease -<br />
Glucose + Soluble Starch + Galactitol - 0.1% Cycloheximide +<br />
Galactose + D-Xylose v D-Mannitol + Growth at 40 O C +<br />
Key Features: germ tube positive, similar to C. albicans, except for absence of growth<br />
at 45 o C; glycerol (mostly +), methyl-α-D-glucoside (-), trehalose (-), and D-xylose (-).<br />
Initial colonies dark green colour on CHROMagar and producing rough colonies on<br />
bird seed agar. C. dubliniensis is an uncommon cause of candidemia and mucosal<br />
infection, especially in HIV patients. RG-2 organism.<br />
Antifungal<br />
MIC µg/mL<br />
MIC µg/mL<br />
Range MIC90 Antifungal Range MIC90 Fluconazole 0.05->64 1 Amphotericin B 0.03-2 0.125<br />
Itraconazole 0.008->8 0.125 Flucytosine 0.03-64 0.125<br />
Posaconazole 0.03-1 0.125 Caspofungin 0.008-1 0.25<br />
Voriconazole 0.008-2 0.016 Anidulafungin
26<br />
Descriptions of Medical Fungi<br />
Candida fabianii (Hartmann) S.A. Meyer & Yarrow<br />
Teleomorph: Pichia fabianii (Wickerham) Kurtzman<br />
Culture: Colonies (SDA) white to cream-coloured smooth, glabrous yeast-like.<br />
Microscopy: Spheroidal to ellipsoidal budding blastoconidia, 3.0-6.5 x 2-5.5 µm in<br />
size. No pseudohyphae produced. Asci when present spherical, containing 1-4 spherical,<br />
faintly roughened ascospores.<br />
India Ink Preparation: Negative - No capsules present.<br />
Dalmau Plate Culture on Cornmeal and Tween 80 Agar: Spherical to ovoid budding<br />
yeast cells and occasional pseudohyphae produced.<br />
Physiological Tests: + Positive, - Negative, v Variable, w Weak, s Slow<br />
Germ Tube - L-Sorbose - L-Arabinose - D-Glucitol +<br />
Fermentation Sucrose + D-Arabinose - α-M-D-glucoside +<br />
Glucose + Maltose + D-Ribose - D-Gluconate +<br />
Galactose - Cellobiose + L-Rhamnose - DL-Lactate +<br />
Sucrose + Trehalose + D-Glucosamine - myo-Inositol -<br />
Maltose +,s Lactose - N-A-D-glucosamine - 2-K-D-gluconate -<br />
Lactose - Melibiose - Glycerol + D-Glucuronate -<br />
Trehalose - Raffinose + Erythritol - Nitrate +<br />
Assimilation Melezitose + Ribitol - Urease -<br />
Glucose + Soluble Starch + Galactitol - 0.1% Cycloheximide -<br />
Galactose - D-Xylose + D-Mannitol + Growth at 37 O C +<br />
Key Features: germ tube negative yeast and sugar assimilation pattern. Molecular<br />
identification may be required. Candida fabianii is a rare cause of candidemia. RG-1<br />
organism.<br />
Antifungal<br />
MIC µg/mL<br />
MIC µg/mL<br />
Antifungal<br />
Range Range<br />
Fluconazole 8 Amphotericin B 0.125<br />
Itraconazole 0.5 Flucytosine 0.03<br />
Posaconazole 0.5 Caspofungin 0.5<br />
Voriconazole 0.125 Anidulafungin nd<br />
Very limited data, antifungal susceptibility testing of individual strains is recommended.<br />
Data from the Australian Candidemia Study (nd = not done).
Descriptions of Medical Fungi 27<br />
Teleomorph: Debaryomyces hansenii (Zopf) Lodder & Kreger-van Rij.<br />
Culture: Colonies (SDA) white to cream-coloured smooth, glabrous yeast-like.<br />
Microscopy: Ovoid to broadly ellipsoidal budding blastoconidia, 3.5-5 x 2-3.5 µm in<br />
size. No pseudohyphae produced. Asci when present spherical, persistent, containing<br />
1-2 spherical ascospores with rough walls.<br />
India Ink Preparation: Negative - No capsules present.<br />
Dalmau Plate Culture on Cornmeal and Tween 80 Agar: Spherical to ovoid budding<br />
yeast cells only. No pseudohyphae produced.<br />
Key Features: germ tube negative yeast and sugar assimilation pattern. Candida<br />
famata is a common environmental isolate, however it is only rarely recovered from<br />
clinical specimens, usually associated with skin. RG-1 organism.<br />
Antifungal<br />
Candida famata (Harrison) S.A. Meyer & Yarrow<br />
Physiological Tests: + Positive, - Negative, v Variable, w Weak, s Slow<br />
Germ Tube - L-Sorbose v L-Arabinose +,w D-Glucitol +,w<br />
Fermentation Sucrose + D-Arabinose v α-M-D-glucoside +<br />
Glucose -,w Maltose + D-Ribose v D-Gluconate +,w<br />
Galactose -,w Cellobiose + L-Rhamnose v DL-Lactate v<br />
Sucrose -,w Trehalose + D-Glucosamine v myo-Inositol -<br />
Maltose - Lactose v N-A-D-glucosamine v 2-K-D-gluconate +<br />
Lactose - Melibiose v Glycerol + D-Glucuronate v<br />
Trehalose -,w Raffinose + Erythritol v Nitrate -<br />
Assimilation Melezitose v Ribitol + Urease -<br />
Glucose + Soluble Starch v Galactitol v 0.1% Cycloheximide v<br />
Galactose + D-Xylose + D-Mannitol + Growth at 40 O C +,w<br />
MIC µg/mL<br />
MIC µg/mL<br />
Range Antifungal<br />
Range<br />
Fluconazole 0.125->64 Amphotericin B 0.06-2<br />
Itraconazole 0.03->8 Flucytosine 0.06-128<br />
Posaconazole 0.06-1 Caspofungin 0.06->16<br />
Voriconazole 0.03-1 Anidulafungin 0.008->16<br />
Limited data, antifungal susceptibility testing of individual strains is recommended.<br />
Espinel-Ingroff et al. (2001), Pfaller et al. (2003, 2007), Espinel-Ingroff (2003),<br />
Cuenca-Estrella et al. (2006) and the Australian Candidemia Study.
28<br />
Descriptions of Medical Fungi<br />
Synonym: Torulopsis glabrata (Anderson) Lodder & de Vries<br />
Culture: Colonies (SDA) white to cream-coloured smooth, glabrous yeast-like.<br />
Microscopy: Ovoid to ellipsoidal budding blastoconidia, 3.4 x 2.0 µm in size. No pseudohyphae<br />
or chlamydospores produced.<br />
India Ink Preparation: Negative - No capsules present.<br />
Dalmau Plate Culture on Cornmeal and Tween 80 Agar: Ovoid budding yeast cells<br />
only. No pseudohyphae produced.<br />
Key Features: germ tube negative yeast and sugar assimilation pattern. Candida glabrata<br />
is one of the most common yeast species to be found on the body surface and<br />
is often isolated as an incidental finding from skin and urine. It has been implicated<br />
as an “opportunistic” cause of both superficial and systemic infections, especially in<br />
immunocompromised patients, and it has been isolated from patients with septicemia,<br />
pyelonephritis, pulmonary infections, endocarditis and hyperalimentation. Approximately<br />
10% of clinical isolates show azole cross resistance. RG-2 organism.<br />
Antifungal<br />
Candida glabrata (Anderson) S.A. Meyer & Yarrow<br />
Physiological Tests: + Positive, - Negative, v Variable, w Weak, s Slow<br />
Germ Tube - L-Sorbose - L-Arabinose - D-Glucitol -<br />
Fermentation Sucrose - D-Arabinose - α-M-D-glucoside -<br />
Glucose + Maltose - D-Ribose - D-Gluconate -<br />
Galactose - Cellobiose - L-Rhamnose - DL-Lactate -<br />
Sucrose - Trehalose - D-Glucosamine - myo-Inositol -<br />
Maltose - Lactose - N-A-D-glucosamine - 2-K-D-gluconate v<br />
Lactose - Melibiose - Glycerol +,s D-Glucuronate -<br />
Trehalose v Raffinose - Erythritol - Nitrate -<br />
Assimilation Melezitose - Ribitol - Urease -<br />
Glucose + Soluble Starch - Galactitol - 0.1% Cycloheximide -<br />
Galactose - D-Xylose - D-Mannitol - Growth at 40 O C +<br />
MIC µg/mL<br />
MIC µg/mL<br />
Range MIC90 Antifungal Range MIC90 Fluconazole 0.03->128 128 Amphotericin B 0.008-2 0.5<br />
Itraconazole 0.008->16 16 Flucytosine 0.008-16 0.03<br />
Posaconazole 0.008-8 8 Caspofungin 0.008->8 0.25<br />
Voriconazole 0.008-16 2 Anidulafungin 0.008-8 nd<br />
Good data available. Espinel-Ingroff et al. (2001), Pfaller et al. (2002b, 2006, 2007),<br />
Espinel-Ingroff (2003), Hajjeh et al. (2004), Richter et al. (2005) and Cuenca-Estrella<br />
et al. (2006). MIC 90 s from the Australian Candidemia Study (note: in this study 10%<br />
of primary blood isolates were azole cross-resistant, nd = not done).
Descriptions of Medical Fungi 29<br />
Teleomorph: Pichia guilliermondii Wickerham.<br />
Culture: White to cream-coloured smooth, glabrous yeast-like colonies.<br />
Microscopy: Spherical to subspherical budding yeast-like cells or blastoconidia, 2.0-<br />
4.0 x 3.0-6.5 µm.<br />
India Ink Preparation: Negative - No capsules present.<br />
Dalmau Plate Culture on Cornmeal and Tween 80 Agar: Branched pseudohyphae<br />
with dense verticils of blastoconidia.<br />
Antifungal<br />
Candida guilliermondii (Castellani) Langeron & Guerra<br />
Physiological Tests: + Positive, - Negative, v Variable, w Weak, s Slow<br />
Germ Tube - L-Sorbose v L-Arabinose v D-Glucitol v<br />
Fermentation Sucrose + D-Arabinose v α-M-D-glucoside v<br />
Glucose + Maltose + D-Ribose + D-Gluconate v<br />
Galactose v Cellobiose v L-Rhamnose v DL-Lactate v<br />
Sucrose + Trehalose + D-Glucosamine + myo-Inositol -<br />
Maltose - Lactose - N-A-D-glucosamine + 2-K-D-gluconate +<br />
Lactose - Melibiose v Glycerol + D-Glucuronate -<br />
Trehalose + Raffinose + Erythritol - Nitrate -<br />
Assimilation Melezitose v Ribitol + Urease -<br />
Glucose + Soluble Starch - Galactitol v 0.1% Cycloheximide v<br />
Galactose + D-Xylose + D-Mannitol v Growth at 37 O C v<br />
Key Features: germ tube negative yeast and sugar assimilation pattern. Candida<br />
guilliermondii has been isolated from numerous human infections, mostly of cutaneous<br />
origin. It is also found from normal skin and in sea water, faeces of animals, fig wasps,<br />
buttermilk, leather, fish, and beer. RG-1 organism.<br />
MIC µg/mL<br />
MIC µg/mL<br />
Range MIC90 Antifungal Range MIC90 Fluconazole 0.125->128 16 Amphotericin B 0.03-1 0.5<br />
Itraconazole 0.03-8 1.0 Flucytosine 0.03-8 0.125<br />
Posaconazole 0.03-8 0.5 Caspofungin 0.125->8 0.5<br />
Voriconazole 0.03-8 0.25 Anidulafungin 0.06-4 nd<br />
Good data available. Espinel-Ingroff et al. (2001), Pfaller et al. (2003, 2006, 2007),<br />
Espinel-Ingroff (2003) and Cuenca-Estrella et al. (2006). MIC 90 s from the Australian<br />
Candidemia Study (nd = not done).
30<br />
Descriptions of Medical Fungi<br />
Candida haemulonii (van Uden & Kolipinski) Meyer & Yarrow<br />
Synonym: Torulopsis haemulonii van Uden & Kolipinski<br />
Culture: Colonies (SDA) white to cream-coloured smooth, glabrous yeast-like.<br />
Microscopy: Ovoid to globose, budding yeast-like cells or blastoconidia, 3.0-5.0 x<br />
3.0-6.5 µm. No pseudohyphae produced.<br />
India Ink Preparation: Negative - No capsules present.<br />
Dalmau Plate Culture on Cornmeal and Tween 80 Agar: Spherical to ovoid, budding<br />
yeast-like cells only. No pseudohyphae produced.<br />
Physiological Tests: + Positive, - Negative, v Variable, w Weak, s Slow<br />
Germ Tube - L-Sorbose - L-Arabinose -,s D-Glucitol +<br />
Fermentation Sucrose + D-Arabinose -,s α-M-D-glucoside -<br />
Glucose + Maltose + D-Ribose -,s D-Gluconate +<br />
Galactose - Cellobiose - L-Rhamnose +,s DL-Lactate -<br />
Sucrose + Trehalose + D-Glucosamine +,s myo-Inositol -<br />
Maltose - Lactose - N-A-D-glucosamine + 2-K-D-gluconate +<br />
Lactose - Melibiose - Glycerol +,s D-Glucuronate -<br />
Trehalose +,s Raffinose +,s Erythritol - Nitrate -<br />
Assimilation Melezitose +,s Ribitol s Urease -<br />
Glucose + Soluble Starch v Galactitol -,s 0.1% Cycloheximide +<br />
Galactose -,s D-Xylose -,s D-Mannitol + Growth at 37 O C +<br />
Key Features: germ tube negative yeast and sugar assimilation pattern. Molecular<br />
identification may be required. Candida haemulonii has been reported from a few<br />
cases of fungemia but clinical isolations remain rare. It has also been isolated from<br />
fish and a dolphin. C. haemulonii may be difficult to distinguish from C. famata using<br />
some commercial yeast identification systems due to data base limitations. RG-1 organism.<br />
Antifungal<br />
MIC µg/mL<br />
MIC µg/mL<br />
Range<br />
Antifungal<br />
Range<br />
Fluconazole 32->256 Amphotericin B 2-8<br />
Itraconazole 0.125-4 Flucytosine 0.008-0.125<br />
Voriconazole 0.06-0.5 Caspofungin 0.03-0.5<br />
Very limited data, antifungal susceptibility testing of individual strains is recommended.<br />
Rodero et al. (2002) and Khan et al. (2007).
Descriptions of Medical Fungi 31<br />
Candida inconspicua (Lodder & Kreger-van Rij) S.A.Meyer & Yarrow<br />
Synonym: Torulopsis inconspicua Lodder & Kreger-van Rij.<br />
Culture: Colonies (SDA) white to cream-coloured smooth, glabrous yeast-like.<br />
Microscopy: Ovoidal budding blastoconidia, 2.0-5 x 5.0-11.0 µm.<br />
India Ink Preparation: Negative - No capsules present.<br />
Dalmau Plate Culture on Cornmeal and Tween 80 Agar: Spherical to ovoid budding<br />
yeast cells only. Primitive pseudohyphae may be produced after 14 days.<br />
Physiological Tests: + Positive, - Negative, v Variable, w Weak, s Slow<br />
Germ Tube - L-Sorbose - L-Arabinose - D-Glucitol -<br />
Fermentation Sucrose - D-Arabinose - α-M-D-glucoside -<br />
Glucose - Maltose - D-Ribose - D-Gluconate -<br />
Galactose - Cellobiose - L-Rhamnose - DL-Lactate +<br />
Sucrose - Trehalose - D-Glucosamine + myo-Inositol -<br />
Maltose - Lactose - N-A-D-glucosamine + 2-K-D-gluconate -<br />
Lactose - Melibiose - Glycerol + D-Glucuronate -<br />
Trehalose - Raffinose - Erythritol - Nitrate -<br />
Assimilation Melezitose - Ribitol - Urease -<br />
Glucose + Soluble Starch - Galactitol - 0.1% Cycloheximide -<br />
Galactose - D-Xylose - D-Mannitol - Growth at 40 O C +<br />
Key Features: germ tube negative yeast and sugar assimilation pattern. Candida<br />
inconspicua is a rare cause of candidemia. RG-1 organism.<br />
Antifungal<br />
MIC µg/mL<br />
MIC µg/mL<br />
Range Antifungal<br />
Range<br />
Fluconazole 4-128 Amphotericin B 0.125->8<br />
Itraconazole 0.25-8 Flucytosine 1-64<br />
Posaconazole 0.5-8 Caspofungin 0.008-0.25<br />
Voriconazole 0.125-4 Anidulafungin nd<br />
Very limited data, antifungal susceptibility testing of individual strains is recommended.<br />
Pfaller et al. (2003), Espinel-Ingroff (2003) and the Australian Candidemia Study (nd<br />
= not done).
32<br />
Descriptions of Medical Fungi<br />
Synonym: Candida pseudotropicalis (Castellani) Basgal.<br />
Teleomorph: Kluyveromyces marxianus (Hansen) van der Walt.<br />
Culture: Colonies (SDA) white to cream-coloured smooth, glabrous yeast-like.<br />
Microscopy: Short-ovoid to long-ovoid, budding blastoconidia, 3.0-6.5 x 5.5-11.0 µm,<br />
sometimes becoming elongate (up to 16.0 µm).<br />
India Ink Preparation: Negative - No capsules present.<br />
Dalmau Plate Culture on Cornmeal and Tween 80 Agar: Abundant, long, wavy,<br />
branched pseudohyphae usually formed, with ovoid blastoconidia, budding off singly,<br />
in pairs or chains, often in a verticillated position. Note: in some strains pseudohyphae<br />
may be scarce or almost absent.<br />
Key Features: germ tube negative yeast and sugar assimilation pattern. Candida<br />
kefyr is a rare cause of candidiasis and is usually associated with superficial cutaneous<br />
manifestations rather than systemic disease. Environmental isolations have been<br />
made from cheese and dairy products. RG-1 organism.<br />
Antifungal<br />
Candida kefyr (Beijerinck) van Uden & Buckley<br />
Physiological Tests: + Positive, - Negative, v Variable, w Weak, s Slow<br />
Germ Tube - L-Sorbose v L-Arabinose v D-Glucitol v<br />
Fermentation Sucrose + D-Arabinose - α-M-D-glucoside -<br />
Glucose + Maltose - D-Ribose v D-Gluconate -<br />
Galactose +,s Cellobiose v L-Rhamnose - DL-Lactate +<br />
Sucrose + Trehalose -,w D-Glucosamine - myo-Inositol -<br />
Maltose - Lactose v N-A-D-glucosamine - 2-K-D-gluconate -<br />
Lactose v Melibiose - Glycerol s D-Glucuronate -<br />
Trehalose - Raffinose + Erythritol - Nitrate -<br />
Assimilation Melezitose - Ribitol s Urease -<br />
Glucose + Soluble Starch - Galactitol - 0.1% Cycloheximide +<br />
Galactose s D-Xylose s D-Mannitol v Growth at 40 O C +<br />
MIC µg/mL<br />
MIC µg/mL<br />
Range MIC90 Antifungal Range MIC90 Fluconazole 0.125-4 0.5 Amphotericin B 0.125->8 1<br />
Itraconazole 0.03-0.5 0.06 Flucytosine 0.03-64 16<br />
Posaconazole 0.03-0.25 0.25 Caspofungin 0.03-1 0.125<br />
Voriconazole 0.008-0.125 0.016 Anidulafungin 0.03-0.5 nd<br />
Limited data, antifungal susceptibility testing of individual strains is recommended.<br />
Espinel-Ingroff et al. (2001), Pfaller et al. (2003, 2006), Espinel-Ingroff (2003) and<br />
Cuenca-Estrella et al. (2006). MIC 90 s from the Australian Candidemia Study (nd =<br />
not done).
Descriptions of Medical Fungi 33<br />
Teleomorph: Issatchenkia orientalis Kudryavtesev.<br />
Culture: Colonies (SDA) white to cream-coloured smooth, glabrous yeast-like.<br />
Microscopy: Predominantly small, elongated to ovoid budding blastoconidia, 2.0-5.5<br />
x 4.0-15.0 µm.<br />
India Ink Preparation: Negative - No capsules present.<br />
Dalmau Plate Culture on Cornmeal and Tween 80 Agar: Abundant long, wavy,<br />
branched pseudohyphae with elongated to ovoid blastoconidia, budding off in verticillate<br />
branches.<br />
Key Features: germ tube negative yeast and sugar assimilation pattern. Candida<br />
krusei is regularly associated with some forms of infant diarrhoea and occasionally<br />
with systemic disease. It has also been reported to colonise the gastrointestinal, respiratory<br />
and urinary tracts of patients with granulocytopenia. Environmental isolations<br />
have been made from beer, milk products, skin, faeces of animals and birds and pickle<br />
brine. RG-2 organism.<br />
Antifungal<br />
Candida krusei (Castellani) Berkhout<br />
Physiological Tests: + Positive, - Negative, v Variable, w Weak, s Slow<br />
Germ Tube - L-Sorbose - L-Arabinose - D-Glucitol -<br />
Fermentation Sucrose - D-Arabinose - α-M-D-glucoside -<br />
Glucose + Maltose - D-Ribose - D-Gluconate -<br />
Galactose - Cellobiose - L-Rhamnose - DL-Lactate +<br />
Sucrose - Trehalose - D-Glucosamine + myo-Inositol -<br />
Maltose - Lactose - N-A-D-glucosamine + 2-K-D-gluconate -<br />
Lactose - Melibiose - Glycerol + D-Glucuronate -<br />
Trehalose - Raffinose - Erythritol - Nitrate -<br />
Assimilation Melezitose - Ribitol - Urease -<br />
Glucose + Soluble Starch - Galactitol - 0.1% Cycloheximide v<br />
Galactose - D-Xylose - D-Mannitol - Growth at 40 O C +<br />
MIC µg/mL<br />
MIC µg/mL<br />
Range MIC90 Antifungal Range MIC90 Fluconazole 0.25->128 64 Amphotericin B 0.06->8 1<br />
Itraconazole 0.03->8 0.5 Flucytosine 0.5-64 16<br />
Posaconazole 0.03-1 1 Caspofungin 0.125->4 1<br />
Voriconazole 0.03-4 0.5 Anidulafungin 0.008-8 nd<br />
Good data available. Espinel-Ingroff et al. (2001), Pfaller et al. (2002b, 2003, 2007),<br />
Espinel-Ingroff (2003), Hajjeh et al. (2004), Richter et al. (2005) and Cuenca-Estrella<br />
et al. (2006). MIC 90 s from the Australian Candidemia Study (nd = not done).
34<br />
Descriptions of Medical Fungi<br />
Candida lipolytica (F.C. Harrison) Diddens & Lodder<br />
Teleomorph: Yarrowia lipolytica (Wickerham et al.) van der Walt & von Arx.<br />
Culture: Colonies (SDA) white to cream-coloured smooth, glabrous yeast-like.<br />
Microscopy: Spherical, ellipsoidal to elongate budding blastoconidia, 3.0-5 x 3.3-15.0<br />
µm.<br />
India Ink Preparation: Negative - No capsules present.<br />
Dalmau Plate Culture on Cornmeal and Tween 80 Agar: Pseudohyphae and true<br />
hyphae are produced.<br />
Physiological Tests: + Positive, - Negative, v Variable, w Weak, s Slow<br />
Germ Tube - L-Sorbose v L-Arabinose - D-Glucitol +<br />
Fermentation Sucrose - D-Arabinose - α-M-D-glucoside -<br />
Glucose - Maltose - D-Ribose v D-Gluconate v<br />
Galactose - Cellobiose w,- L-Rhamnose - DL-Lactate +<br />
Sucrose - Trehalose - D-Glucosamine - myo-Inositol -<br />
Maltose - Lactose - N-A-D-glucosamine + 2-K-D-gluconate -<br />
Lactose - Melibiose - Glycerol + D-Glucuronate -<br />
Trehalose - Raffinose - Erythritol + Nitrate -<br />
Assimilation Melezitose - Ribitol v Urease -<br />
Glucose + Soluble Starch - Galactitol - 0.1% Cycloheximide -<br />
Galactose v D-Xylose - D-Mannitol + Growth at 37 O C v<br />
Key Features: germ tube negative yeast and sugar assimilation pattern. Candida<br />
lipolytica is a rare cause of candidemia. RG-1 organism.<br />
Antifungal<br />
MIC µg/mL<br />
MIC µg/mL<br />
Range Antifungal<br />
Range<br />
Fluconazole 1->64 Amphotericin B 0.06-1<br />
Itraconazole 0.06-8 Flucytosine 0.125-64<br />
Posaconazole 0.03-4 Caspofungin 0.25-2<br />
Voriconazole 0.03-1 Anidulafungin 0.125-0.5<br />
Limited data, antifungal susceptibility testing of individual strains is recommended.<br />
Espinel-Ingroff et al. (2001), Pfaller et al. (2003), Espinel-Ingroff (2003) and Australian<br />
Candidemia Study.
Descriptions of Medical Fungi 35<br />
Candida lusitaniae van Uden & do Carmo-Sousa<br />
Teleomorph: Clavispora lusitaniae Rodrigues de Miranda.<br />
Culture: Colonies (SDA) white to cream-coloured smooth, glabrous yeast-like.<br />
Microscopy: Ovoid to ellipsoidal budding blastoconidia, 1.5-6.0 x 2.5-10.0 µm.<br />
India Ink Preparation: Negative - No capsules present.<br />
Dalmau Plate Culture on Cornmeal and Tween 80 Agar: Abundant pseudohyphae<br />
with short chains of blastoconidia.<br />
Physiological Tests: + Positive, - Negative, v Variable, w Weak, s Slow<br />
Germ Tube - L-Sorbose + L-Arabinose v D-Glucitol +<br />
Fermentation Sucrose + D-Arabinose - α-M-D-glucoside v<br />
Glucose + Maltose + D-Ribose - D-Gluconate s<br />
Galactose v Cellobiose + L-Rhamnose v DL-Lactate +,w<br />
Sucrose v Trehalose + D-Glucosamine - myo-Inositol -<br />
Maltose v Lactose - N-A-D-glucosamine + 2-K-D-gluconate +<br />
Lactose - Melibiose - Glycerol + D-Glucuronate -<br />
Trehalose v Raffinose - Erythritol - Nitrate -<br />
Assimilation Melezitose + Ribitol s Urease -<br />
Glucose + Soluble Starch - Galactitol - 0.1% Cycloheximide -<br />
Galactose + D-Xylose + D-Mannitol + Growth at 40 O C +<br />
Key Features: germ tube negative yeast and sugar assimilation pattern. Candida<br />
lusitaniae is a known cause of disseminated candidiasis, including septicemia and<br />
pyelonephritis. C. lusitaniae was first isolated from the alimentary tract of warm blooded<br />
animals and environmental isolations have been made from cornmeal, citrus peel,<br />
fruit juices, and milk from cows with mastitis. C. lusitaniae may also be difficult to distinguish<br />
from C. tropicalis using some yeast identification systems. RG-2 organism.<br />
Antifungal<br />
MIC µg/mL<br />
MIC µg/mL<br />
Range MIC90 Antifungal Range MIC90 Fluconazole 0.125-64 8 Amphotericin B 0.03-8 0.125<br />
Itraconazole 0.06-2 0.125 Flucytosine 0.03-128 0.03<br />
Posaconazole 0.008-0.5 0.25 Caspofungin 0.125-4 0.5<br />
Voriconazole 0.008-2 0.125 Anidulafungin 0.03->8 nd<br />
Some data available. Espinel-Ingroff et al. (2001), Pfaller et al. (2002b, 2003),<br />
Espinel-Ingroff (2003) and Cuenca-Estrella et al. (2006). MIC 90 s from the Australian<br />
Candidemia Study (nd = not done).
36<br />
Descriptions of Medical Fungi<br />
Candida norvegensis Dietrichson ex van Uden & Buckley<br />
Teleomorph: Pichia norvegensis Leask & Yarrow.<br />
Culture: Colonies (SDA) white to cream-coloured smooth, glabrous yeast-like.<br />
Microscopy: Ovoid, budding blastoconidia, 2.0-3.5 x 3.5-5.0 µm. Pseudohyphae<br />
rarely produced.<br />
India Ink Preparation: Negative - No capsules present.<br />
Dalmau Plate Culture on Cornmeal and Tween 80 Agar: Spherical to ovoid budding<br />
yeast cells only. No pseudohyphae produced.<br />
Physiological Tests: + Positive, - Negative, v Variable, w Weak, s Slow<br />
Germ Tube - L-Sorbose - L-Arabinose - D-Glucitol -<br />
Fermentation Sucrose - D-Arabinose - α-M-D-glucoside -<br />
Glucose s Maltose - D-Ribose - D-Gluconate -<br />
Galactose - Cellobiose + L-Rhamnose - DL-Lactate w<br />
Sucrose - Trehalose - D-Glucosamine + myo-Inositol -<br />
Maltose - Lactose - N-A-D-glucosamine - 2-K-D-gluconate -<br />
Lactose - Melibiose - Glycerol + D-Glucuronate -<br />
Trehalose - Raffinose - Erythritol - Nitrate -<br />
Assimilation Melezitose - Ribitol - Urease -<br />
Glucose + Soluble Starch - Galactitol - 0.1% Cycloheximide -<br />
Galactose - D-Xylose - D-Mannitol - Growth at 37 O C +<br />
Key Features: germ tube negative yeast and sugar assimilation pattern. Candida<br />
norvegensis is a very rare clinical isolate that has been reported as a causative agent<br />
of peritonitis and disseminated candidiasis in a patient on CAPD. RG-1 organism.<br />
Antifungal<br />
MIC µg/mL<br />
MIC µg/mL<br />
Range<br />
Antifungal<br />
Range<br />
Fluconazole 16 Amphotericin B 1<br />
Itraconazole 0.25 Flucytosine 8<br />
Voriconazole 0.125 Posaconazole 0.125<br />
Very limited data, antifungal susceptibility testing of individual strains is recommended.<br />
Pfaller et al. (2002b).
Descriptions of Medical Fungi 37<br />
Candida parapsilosis Complex<br />
Recently Candida parapsilosis has been recognised as 3 species: C. parapsilosis, C.<br />
orthopsilosis and C. metapsilosis (Tavanti et al. 2005). These three species are phenotypically<br />
indistinguishable and are best distinguished by genetic analysis. Antifungal<br />
susceptibility data from the Australian Candidemia Study also shows no significant differences<br />
between the species.<br />
Culture: Colonies (SDA) white to cream-coloured smooth, glabrous yeast-like.<br />
Microscopy: Predominantly small, globose to ovoid budding blastoconidia, 2.0-3.5 x<br />
3.0-4.5 µm, with some larger elongated forms present.<br />
India Ink Preparation: Negative - No capsules present.<br />
Dalmau Plate Culture on Cornmeal and Tween 80 Agar: Abundant, much-branched<br />
pseudohyphae in a delicate tree-like pattern with 2-3 blastoconidia in small clusters at<br />
intervals along the pseudohyphae.<br />
Physiological Tests: + Positive, - Negative, v Variable, w Weak, s Slow<br />
Germ Tube - L-Sorbose +,s L-Arabinose + D-Glucitol +<br />
Fermentation Sucrose + D-Arabinose - α-M-D-glucoside +<br />
Glucose + Maltose + D-Ribose v D-Gluconate +,s<br />
Galactose v Cellobiose - L-Rhamnose - DL-Lactate -<br />
Sucrose -,s Trehalose + D-Glucosamine v myo-Inositol -<br />
Maltose -,s Lactose - N-A-D-glucosamine + 2-K-D-gluconate +<br />
Lactose - Melibiose - Glycerol + D-Glucuronate -<br />
Trehalose -,s Raffinose - Erythritol - Nitrate -<br />
Assimilation Melezitose + Ribitol +,s Urease -<br />
Glucose + Soluble Starch - Galactitol - 0.1% Cycloheximide -<br />
Galactose + D-Xylose + D-Mannitol + Growth at 37 O C +<br />
Key Features: germ tube negative yeast and sugar assimilation pattern. Candida<br />
parapsilosis is an opportunistic human pathogen which may cause cutaneous infections,<br />
especially of the nail and systemic disease, especially endocarditis. Other clinical<br />
manifestations include endophthalmitis and fungemia. Environmental isolations have<br />
been made from intertidal and oceanic waters, pickle brine, cured meats, olives and<br />
normal skin, and faeces. RG-1 organism.<br />
Antifungal<br />
MIC µg/mL<br />
MIC µg/mL<br />
Range MIC90 Antifungal Range MIC90 Fluconazole 0.125->64 8 Amphotericin B 0.016-2 0.5<br />
Itraconazole 0.015-2 0.25 Flucytosine 0.03->64 0.25<br />
Posaconazole 0.008-0.5 0.03 Caspofungin 0.03->8 1<br />
Voriconazole 0.008-2 0.25 Anidulafungin 0.008->8 nd<br />
Good data available. Espinel-Ingroff et al. (2001), Pfaller et al. (2002b, 2006, 2007),<br />
Espinel-Ingroff (2003), Hajjeh et al. (2004), Richter et al. (2005) and Cuenca-Estrella<br />
et al. (2006). MIC 90 s from the Australian Candidemia Study (nd = not done).
38<br />
Descriptions of Medical Fungi<br />
Candida pelliculosa Redaelli<br />
Teleomorph: Pichia anomala (Hansen) Kurtzman.<br />
Culture: Colonies (SDA) white to cream-coloured smooth, glabrous yeast-like.<br />
Microscopy: Spherical to ellipsoidal budding blastoconidia, 2-4 x 2-6 µm. Pseudohyphae<br />
may be present. Asci when present, containing 1-4 hat-shaped ascospores.<br />
India Ink Preparation: Negative - No capsules present.<br />
Dalmau Plate Culture on Cornmeal and Tween 80 Agar: Spherical to ellipsoidal<br />
budding yeast cells and abundant pseudohyphae in most strains.<br />
Physiological Tests: + Positive, - Negative, v Variable, w Weak, s Slow<br />
Germ Tube - L-Sorbose - L-Arabinose v D-Glucitol +<br />
Fermentation Sucrose + D-Arabinose - α-M-D-glucoside +<br />
Glucose + Maltose + D-Ribose v D-Gluconate v<br />
Galactose v Cellobiose + L-Rhamnose - DL-Lactate +<br />
Sucrose + Trehalose + D-Glucosamine - myo-Inositol -<br />
Maltose v Lactose - N-A-D-glucosamine - 2-K-D-gluconate -<br />
Lactose - Melibiose - Glycerol + D-Glucuronate n<br />
Trehalose - Raffinose + Erythritol + Nitrate +<br />
Assimilation Melezitose + Ribitol v Urease -<br />
Glucose + Soluble Starch + Galactitol - 0.1% Cycloheximide -<br />
Galactose v D-Xylose v D-Mannitol + Growth at 37 O C v<br />
Key Features: germ tube negative yeast and sugar assimilation pattern. Candida<br />
pelliculosa has been reported from cases of candidemia and catheter related infections<br />
in humans and has been isolated from soil, grains, fruit and warm blooded animals.<br />
RG-1 organism.<br />
Antifungal<br />
MIC µg/mL<br />
MIC µg/mL<br />
Range<br />
Antifungal<br />
Range<br />
Fluconazole 2-16 Amphotericin B 0.125-2<br />
Itraconazole 0.25-2 Flucytosine 0.03-64<br />
Posaconazole 0.125-1 Caspofungin 0.06-0.5<br />
Voriconazole 0.06-0.25 Anidulafungin nd<br />
Limited data available, antifungal susceptibility testing of individual strains is<br />
recommended. Pfaller et al. (2003), Espinel-Ingroff (2003), Cuenca-Estrella et al.<br />
(2006) and the Australian Candidemia Study (nd = not done).
Descriptions of Medical Fungi 39<br />
Candida rugosa (Anderson) Diddens & Lodder<br />
Culture: Colonies (SDA) white to cream-coloured smooth, glabrous yeast-like.<br />
Microscopy: Ellipsoidal to elongate budding blastoconidia, 6-10 x 2-3.5 µm. Sometimes<br />
short pseudohyphae may be produced.<br />
India Ink Preparation: Negative - No capsules present.<br />
Dalmau Plate Culture on Cornmeal and Tween 80 Agar: Ellipsoidal budding yeast<br />
cells only and densely branched pseudohyphae produced.<br />
Physiological Tests: + Positive, - Negative, v Variable, w Weak, s Slow<br />
Germ Tube - L-Sorbose v L-Arabinose - D-Glucitol +,s<br />
Fermentation Sucrose - D-Arabinose - α-M-D-glucoside -<br />
Glucose - Maltose - D-Ribose - D-Gluconate v<br />
Galactose - Cellobiose - L-Rhamnose - DL-Lactate +,s<br />
Sucrose - Trehalose - D-Glucosamine - myo-Inositol -<br />
Maltose - Lactose - N-A-D-glucosamine s 2-K-D-gluconate -<br />
Lactose - Melibiose - Glycerol + D-Glucuronate -<br />
Trehalose - Raffinose - Erythritol - Nitrate -<br />
Assimilation Melezitose - Ribitol -,s Urease -<br />
Glucose + Soluble Starch - Galactitol - 0.1% Cycloheximide -<br />
Galactose + D-Xylose v D-Mannitol +,s Growth at 37 O C +<br />
Key Features: germ tube negative yeast and sugar assimilation pattern. Candida<br />
rugosa has been associated with catheter related fungemia and has been isolated<br />
from human and bovine faeces, sea water and soil. RG-1 organism.<br />
Antifungal<br />
MIC µg/mL<br />
MIC µg/mL<br />
Range Antifungal<br />
Range<br />
Fluconazole 1-16 Amphotericin B 0.25-4<br />
Itraconazole 0.03-1 Flucytosine 0.06-16<br />
Posaconazole 0.06-0.25 Caspofungin 0.25-2<br />
Voriconazole 0.008-0.25 Anidulafungin 0.03-4<br />
Limited data, antifungal susceptibility testing of individual strains is recommended.<br />
Espinel-Ingroff et al. (2001), Pfaller et al. (2003), Espinel-Ingroff (2003) and the<br />
Australian Candidemia Study.
40<br />
Descriptions of Medical Fungi<br />
Culture: Colonies (SDA) white to cream-coloured smooth, glabrous yeast-like.<br />
Microscopy: Spherical to subspherical budding yeast-like cells or blastoconidia, 3-5.5<br />
x 4-9 µm.<br />
India Ink Preparation: Negative - No capsules present.<br />
Dalmau Plate Culture on Cornmeal and Tween 80 Agar: Abundant, long, wavy,<br />
branched pseudohyphae with numerous ovoid blastoconidia, budding off. Terminal<br />
vesicles (chlamydospores) are not produced.<br />
Key Features: germ tube negative yeast and sugar assimilation pattern. Candida<br />
tropicalis is a major cause of septicemia and disseminated candidiasis. It is also found<br />
as part of the normal human mucocutaneous flora and environmental isolations have<br />
been made from faeces, shrimp, kefir, and soil. RG-2 organism.<br />
Antifungal<br />
Candida tropicalis (Castellani) Berkhout<br />
Physiological Tests: + Positive, - Negative, v Variable, w Weak, s Slow<br />
Germ Tube - L-Sorbose v L-Arabinose - D-Glucitol +<br />
Fermentation Sucrose v D-Arabinose - α-M-D-glucoside v<br />
Glucose + Maltose + D-Ribose -,s D-Gluconate v<br />
Galactose + Cellobiose +,s L-Rhamnose - DL-Lactate v<br />
Sucrose v Trehalose + D-Glucosamine v myo-Inositol -<br />
Maltose + Lactose - N-A-D-glucosamine + 2-K-D-gluconate +<br />
Lactose - Melibiose - Glycerol v D-Glucuronate -<br />
Trehalose +,s Raffinose - Erythritol - Nitrate -<br />
Assimilation Melezitose v Ribitol +,s Urease -<br />
Glucose + Soluble Starch + Galactitol - 0.1% Cycloheximide +<br />
Galactose + D-Xylose + D-Mannitol + Growth at 40 O C +<br />
MIC µg/mL<br />
MIC µg/mL<br />
Range MIC90 Antifungal Range MIC90 Fluconazole 0.125->128 2 Amphotericin B 0.03-8 0.5<br />
Itraconazole 0.03->8 0.5 Flucytosine 0.03->64 0.125<br />
Posaconazole 0.008->8 0.06 Caspofungin 0.03->8 0.25<br />
Voriconazole 0.008->8 0.25 Anidulafungin 0.03->8 nd<br />
Good data available. Espinel-Ingroff et al. (2001), Pfaller et al. (2002b, 2006, 2007),<br />
Espinel-Ingroff (2003), Hajjeh et al. (2004), Richter et al. (2005) and Cuenca-Estrella<br />
et al. (2006). MIC 90 s from the Australian Candidemia Study (nd = not done).
Descriptions of Medical Fungi 41<br />
Chaetomium Kunze ex Fries<br />
This genus is a common ascomycete (pyrenomycete) characterised by the formation of<br />
darkly-pigmented, globose, ovoid, barrel to flask-shaped, ostiolate ascocarps (perithecia)<br />
beset with dark-coloured terminal hairs (setae) which are straight, branched or<br />
curved. Asci are clavate to cylindrical, typically eight-spored and evanescent. Ascospores<br />
are one-celled, darkly-pigmented, smooth-walled, of varying shape, mostly<br />
ovoid, ellipsoidal or lemon-shaped. Chlamydospores and solitary conidia may also be<br />
produced. RG-1 organism.<br />
The genus contains between 160 and 180 species, and all are saprophytic being isolated<br />
from soil, straw, dung and plant debris. However, quite a few species are thermophilic<br />
and can grow at temperatures above 37 O C. Chaetomium species are important<br />
agents for the decomposition of cellulose waste and plant materials, and are only<br />
rarely isolated in medical mycology laboratories.<br />
Key Features: ascomycete producing darkly-pigmented ostiolate perithecia beset with<br />
long dark terminal setae.<br />
For descriptions of species, keys to taxa and additional information see Ames (1963),<br />
Seth (1970), Millner (1975), Domsch et al. (1980), Ellis and Keane (1981), Ellis (1981)<br />
and de Hoog et al. (2000).<br />
100 μm<br />
10 μm<br />
Ascocarp (perithecia), terminal hairs, asci and ascospores of Chaetomium.<br />
Antifungal<br />
MIC µg/mL MIC µg/mL MIC µg/mL<br />
Antifungal Antifungal<br />
Range Range Range<br />
Amphotericin B 0.125-16 Itraconazole 0.03-0.125 Voriconazole 0.125-0.5<br />
Very limited data, antifungal susceptibility testing of individual strains is recommended.<br />
McGinnis and Pasarell (1998) and WCH in-house data.
42<br />
Descriptions of Medical Fungi<br />
Chrysosporium Corda<br />
Colonies are moderately fast growing, flat, white to tan to beige in colour, often with a<br />
powdery or granular surface texture. Reverse pigment absent or pale brownish-yellow<br />
with age. Hyaline, one-celled conidia are produced directly on vegetative hyphae<br />
by non-specialised conidiogenous cells. Conidia are typically pyriform to clavate with<br />
truncate bases and are formed either intercalary (arthroconidia), laterally (often on<br />
pedicels) or terminally.<br />
Species of Chrysosporium are occasionally isolated from skin and nail scrapings, especially<br />
from feet, but because they are common soil saprophytes they are usually<br />
considered as contaminants. There are about 22 species of Chrysosporium, several<br />
are keratinolytic with some also being thermotolerant, and cultures may closely resemble<br />
some dermatophytes, especially Trichophyton mentagrophytes, and some strains<br />
may also resemble cultures of Histoplasma and Blastomyces.<br />
Chrysosporium tropicum Carmichael<br />
Colonies are flat, white to cream-coloured with a very granular surface. Reverse pigment<br />
absent or pale brownish-yellow with age. Microscopically, conidia are numerous,<br />
hyaline, single-celled, clavate to pyriform, smooth, slightly thick-walled (6-7 x 3.5-4<br />
µm), and have broad truncate bases and pronounced basal scars. The conidia are<br />
formed at the tips of the hyphae, on short or long lateral branches, or sessile along the<br />
hyphae (intercalary). No macroconidia or hyphal spirals are seen. RG-2 organism.<br />
For descriptions of species, keys to taxa and additional information see Carmichael<br />
(1962), Rebell and Taplin (1970), Sigler and Carmichael (1976), Van Oorschot (1980),<br />
Domsch et al. (1980) and de Hoog et al. (2000).<br />
10 μm<br />
Chrysosporium tropicum showing typical pyriform to clavate-shaped conidia<br />
with truncated bases which may be formed either intercalary, laterally<br />
or terminally.
Descriptions of Medical Fungi 43<br />
Cladophialophora bantiana (Saccardo) de Hoog et al.<br />
Synonym: Xylohypha bantiana (Saccardo) McGinnis, Borelli and Ajello<br />
Colonies are moderately fast growing, olivaceous-grey, suede-like to floccose and<br />
grow at temperatures up to 42-43 O C. Conidia are formed in long, sparsely branched,<br />
flexuose, acropetal chains from undifferentiated conidiophores. Conidia are one-celled<br />
(very occasionally two-celled), pale brown, smooth-walled, ellipsoid to oblong-ellipsoid<br />
and are 2-3 x 4-7 µm in size.<br />
Cladophialophora bantiana has been isolated from soil and is a recognised agent of<br />
cerebral phaeohyphomycosis. The fungus is neurotropic and may cause brain abscesses<br />
in both normal and immunosuppressed patients. RG-2 organism.<br />
Cladophialophora bantiana may be distinguished from Cladosporium species by the<br />
absence of conidia with distinctly pigmented hila, the absence of characteristic shield<br />
cells and by growth at 42 O C (compared with Cladophialophora carrionii which has a<br />
maximum growth temperature of 35-36 O C, and Cladosporium species which have a<br />
maximum of less than 35 O C).<br />
For descriptions of species, keys to taxa and additional information see McGinnis<br />
(1980), McGinnis and Borelli (1981), McGinnis et al. (1986a), Rippon (1988), Kwon-<br />
Chung and Bennett (1992) and de Hoog et al. (2000).<br />
10 μm<br />
Conidiophore and conidia of Cladophialophora bantiana.<br />
Antifungal<br />
MIC µg/mL<br />
Range MIC90 Antifungal<br />
MIC µg/mL<br />
Range MIC90 Amphotericin B 0.03-2 0.5 Posaconazole 0.008-0.06 0.06<br />
Itraconazole 0.03-0.5 0.5 Voriconazole 0.03-1 0.125<br />
Limited data, antifungal susceptibility testing of individual strains is recommended.<br />
McGinnis and Pasarell (1998), Espinel-Ingroff et al. (2001), Espinel-Ingroff (2001)<br />
and WCH in-house data.
44<br />
Descriptions of Medical Fungi<br />
Cladophialophora carrionii (Trejos) de Hoog et al.<br />
Synonym: Cladosporium carrionii Trejos<br />
Colonies are slow growing, reaching 3-4 cm in diameter after one month, with a compact<br />
suede-like to downy surface and are olivaceous-black in colour. Microscopy shows<br />
ascending to erect, olivaceous-green, apically branched, elongate conidiophores<br />
producing branched acropetal chains of smooth-walled conidia. Conidia are pale<br />
olivaceous, smooth-walled or slightly verrucose, limoniform to fusiform, 1.5-3.0 x 2.0-<br />
7.0 µm in size. Bulbous phialides with large collarettes and minute, hyaline conidia<br />
are occasionally formed on nutritionally poor media. Maximum growth temperature<br />
35-37 O C. RG-2 organism.<br />
Cladophialophora carrionii is a recognised agent of chromoblastomycosis and it<br />
has been isolated from soil and fence posts made from Eucalyptus sp. Cases of<br />
chromoblastomycosis caused by C. carrionii are commonly found in Australia,<br />
Venezuela, Madagascar and South America. Isolates from phaeomycotic cysts and<br />
opportunistic infections have also been reported.<br />
Key Features: conidia are smaller and comprise heavily branched systems which fall<br />
apart much more easily than in the other Cladophialophora species.<br />
For descriptions of species, keys to taxa and additional information see McGinnis<br />
(1980), Rippon (1988), de Hoog et al. (1995) and de Hoog et al. (2000).<br />
10 μm<br />
Conidiophores and conidia of Cladophialophora carrionii.<br />
Antifungal<br />
MIC µg/mL<br />
Range MIC90 Antifungal<br />
MIC µg/mL<br />
Range MIC90 Amphotericin B 0.06-4 1 Posaconazole 0.06-0.5 0.25<br />
Itraconazole 0.03-0.5 0.5 Voriconazole 0.03-0.5 0.25<br />
Limited data, antifungal susceptibility testing of individual strains is recommended.<br />
McGinnis and Pasarell (1998), Espinel-Ingroff et al. (2001), Gonzales et al. (2005)<br />
and WCH in-house data.
Descriptions of Medical Fungi 45<br />
Cladosporium Link ex Fries<br />
Colonies are rather slow growing, mostly olivaceous-brown to blackish brown but also<br />
sometimes grey, buff or brown, suede-like to floccose, often becoming powdery due<br />
to the production of abundant conidia. Vegetative hyphae, conidiophores and conidia<br />
are equally pigmented. Conidiophores are more or less distinct from the vegetative<br />
hyphae, being erect, straight or flexuose, unbranched or branched only in the apical<br />
region, with geniculate sympodial elongation in some species. Conidia are produced in<br />
branched acropetal chains, being smooth, verrucose or echinulate, one- to four-celled,<br />
and have a distinct dark hilum. The term blastocatenate is often used to describe<br />
chains of conidia where the youngest conidium is at the apical or distal end of the chain.<br />
Note: the conidia closest to the conidiophore, and where the chains branch, are usually<br />
“shield-shaped”. The presence of shield-shaped conidia, a distinct hilum, and chains<br />
of conidia that readily disarticulate, are diagnostic for the genus Cladosporium.<br />
Cladosporium species have a world-wide distribution and are amongst the most common<br />
of air-borne fungi. Some 500 species have been described. Isolates of Cladosporium<br />
are frequently isolated as contaminants. RG-1 organisms. The pathogenic species<br />
have now been transferred to the genus Cladophialophora.<br />
Key Features: dematiaceous hyphomycete forming branched acropetal chains of<br />
conidia, each with a distinct hilum.<br />
For descriptions of species, keys to taxa and additional information see Ellis (1971 and<br />
1976), Domsch et al. (1980), McGinnis (1980) and de Hoog et al. (2000).<br />
Antifungal<br />
10 μm<br />
Conidiophores and conidia of Cladosporium cladosporioides.<br />
MIC µg/mL MIC µg/mL MIC µg/mL<br />
Antifungal Antifungal<br />
Range Range Range<br />
Amphotericin B 0.03-8 Itraconazole 0.03-32 Voriconazole 0.06-1<br />
Very limited data, antifungal susceptibility testing of individual strains is recommended.<br />
McGinnis and Pasarell (1998) and WCH in-house data.
46<br />
Descriptions of Medical Fungi<br />
Coccidioides immitis/posadasii complex<br />
Recently Coccidioides immitis has been recognised as 2 species: C. immitis and C.<br />
posadasii (Fisher et al. 2002). The two species are morphologically identical and can<br />
be distinguished only by genetic analysis and different rates of growth in the presence<br />
of high salt concentrations (C. posadasii grows more slowly). C. immitis is geographically<br />
limited to California’s San Joaquin Valley region, whereas C. posadasii is found in<br />
the desert regions of the USA southwest, Mexico and South America. The two species<br />
appear to coexist in the desert regions of the USA southwest and Mexico.<br />
Colonies of C. immitis/posadasii on Sabouraud’s dextrose agar at 25 O C are initially<br />
moist and glabrous, but rapidly become suede-like to downy, greyish white with a tan<br />
to brown reverse, however considerable variation in growth rate and culture morphology<br />
has been noted. Microscopy shows typical single-celled, hyaline, rectangular to<br />
barrel-shaped, alternate arthroconidia, 2.5-4 x 3-6 µm in size, separated from each<br />
other by a disjunctor cell. This arthroconidial state has been classified in the genus<br />
Malbranchea and is similar to that produced by many non-pathogenic soil fungi, e.g.<br />
Gymnoascus species.<br />
WARNING: RG-3 organism. Cultures of Coccidioides immitis/posadasii represent a<br />
severe biohazard to laboratory personnel and must be handled with extreme caution in<br />
an appropriate pathogen handling cabinet. C. immitis/posadasii is a dimorphic fungus,<br />
existing in living tissue as spherules and endospores, and in soil or culture in a mycelial<br />
form. Culture identification by exoantigen test is now the method of choice.<br />
Key Features: clinical history, tissue pathology, culture identification by positive<br />
exoantigen test.<br />
20 μm<br />
Tissue morphology showing typical endosporulating spherules of C. immitis. Young<br />
spherules have a clear centre with peripheral cytoplasm and a prominent thick-wall.<br />
Endospores (sporangiospores) are later formed within the spherule by repeated cytoplasmic<br />
cleavage. Rupture of the spherule releases endospores into the surrounding<br />
tissue where they re-initiate the cycle of spherule development.
Descriptions of Medical Fungi 47<br />
Coccidioides immitis/posadasii complex<br />
5 μm<br />
Culture and arthroconidia separated from each other by disjunctor<br />
cells of Coccidioides immitis/posadasii.<br />
For descriptions of species, keys to taxa and additional information see Ajello (1957),<br />
Steele et al. (1977), McGinnis (1980), Chandler et al. (1980), Catanzaro (1986), Rippon<br />
(1988), de Hoog et al. (2000) and Fisher et al. (2002).<br />
Antifungal<br />
MIC µg/mL<br />
Range MIC90 Antifungal<br />
MIC µg/mL<br />
Range MIC90 Amphotericin B 0.06-2 1 Posaconazole 0.03-1 0.5<br />
Fluconazole 2-64 32 Voriconazole 0.03-1 0.5<br />
Itraconazole 0.03-2 0.5<br />
Limited data available. Espinel-Ingroff et al. (2001), Espinel-Ingroff (2003), Gonzalez<br />
et al. (2005) and Sabatelli et al. (2006).
48<br />
Descriptions of Medical Fungi<br />
Colletotrichum coccodes (Wallroth) S. Hughes<br />
Colonies usually darkly pigmented with white aerial mycelium, consisting of numerous<br />
black sclerotia and light brown-coloured conidial masses, reverse is dark brown.<br />
Sclerotia are usually abundant, setose, spherical and are often confluent. Conidia are<br />
straight, fusiform, attenuated at the ends, 16-22 x 3-4 µm. Appressoria are common,<br />
clavate, brown, 11-16.5 x 6-9.5 µm, variable in shape. RG-1 organism.<br />
Over 500 Colletotrichum species have been reported. C. coccodes is a common soil<br />
and plant pathogen widely distributed in Africa, Asia, Australasia, Europe, and the<br />
Americas. It has been reported from a case of human mycotic keratitis.<br />
For descriptions of species, keys to taxa and additional information see Domsch et al.<br />
(1980), McGinnis (1980) and de Hoog et al. (2000).<br />
20 μm<br />
10 μm<br />
50 μm<br />
Sclerotia with setae, conidia and appressoria of C. coccodes.
Descriptions of Medical Fungi 49<br />
Synonym: Entomophthora coronata (Costantin) Kevorkian<br />
The species of the genus Conidiobolus produce characteristic multinucleate primary<br />
and secondary (replicative) conidia on top of unbranched conidiophores. Each subspherical<br />
conidium is discharged as a result of the pressure developed within the conidium,<br />
and each bears a more or less prominent papilla after discharge (King 1983).<br />
The genus contains 27 species, however C. coronatus and C. incongruus are the only<br />
species that are known to cause human disease, although C. lamprauges has also<br />
been reported once from a horse (Humber, Brown and Kornegay, 1989).<br />
Colonies of C. coronatus grow rapidly and are flat, cream-coloured, glabrous becoming<br />
radially folded and covered by a fine, powdery, white surface mycelium and conidiophores.<br />
The lid of the petri dish soon becomes covered with conidia, which are<br />
forcibly discharged by the conidiophores. The colour of the colony may become tan to<br />
brown with age. Conidiophores are simple forming solitary, terminal conidia which are<br />
spherical, 10 to 25 µm in diameter, single-celled and have a prominent papilla. Conidia<br />
may also produce hair-like appendages, called villae. Conidia germinate to produce<br />
either, (1) single or multiple hyphal tubes that may also become conidiophores which<br />
bear secondary conidia, or (2) replicate by producing multiple short conidiophores,<br />
each bearing a small secondary conidium. RG-2 organism.<br />
Conidiobolus coronatus is commonly present in soil and decaying leaves. It has a<br />
world-wide distribution especially tropical rain forests of Africa. Human infections are<br />
usually restricted to the rhinofacial area. However, there are occasional reports of<br />
dissemination to other sites. All human infections have been confined to the tropics.<br />
For descriptions of species, keys to taxa and additional information see Emmons and<br />
Bridges (1961), King (1976a, 1976b, 1983), McGinnis (1980), Rippon (1988), Kwon-<br />
Chung and Bennett (1992), de Hoog et al. (2000) and Ellis (2005a).<br />
10 μm<br />
Conidiobolus coronatus (Costantin) Batko<br />
10 μm<br />
Spherical conidia with hair-like appendages (villae) and prominent papillae<br />
characteristic of Conidiobolus coronatus.
50<br />
Descriptions of Medical Fungi<br />
Cryptococcus Kützing emend. Phaff & Spencer<br />
The genus Cryptococcus is characterised by globose to elongate yeast-like cells or<br />
blastoconidia that reproduce by multilateral budding, by polar budding on a narrow<br />
base (may or may not be present), and pseudohyphae being absent or rudimentary.<br />
Most strains have capsulated cells; extent of capsule formation depends on the medium.<br />
Under certain conditions of growth the capsule may contain starch-like compounds,<br />
which are released into the medium by many strains. On solid media the<br />
cultures are generally mucoid or slimy in appearance; red, orange or yellow carotenoid<br />
pigments may be produced, but young colonies of most species are usually non-pigmented,<br />
being cream in colour. No fermentation: Nitrate assimilated or not: Inositol<br />
assimilated. The genus Cryptococcus is similar to the genus Rhodotorula. The distinctive<br />
difference between the two is the assimilation of inositol, which is positive in<br />
Cryptococcus.<br />
Cryptococcosis is a chronic, subacute to acute pulmonary, systemic or meningitic disease,<br />
initiated by the inhalation of basidiospores and/or desiccated yeast cells of Cryptococcus<br />
species. Primary pulmonary infections have no diagnostic symptoms and<br />
are usually subclinical. On dissemination, the fungus usually shows a predilection for<br />
the central nervous system, however skin, bones and other visceral organs may also<br />
become involved. Although C. neoformans and C. gattii are regarded as the principle<br />
pathogenic species, Cryptococcus albidus and Cryptococcus laurentii have on occasion<br />
also been implicated in human infection.<br />
5 μm<br />
Culture appearances on Bird Seed Agar of Cryptococcus neoformans (brown<br />
colonies) and Candida albicans (white colonies) and India ink preparation of<br />
C. neoformans surrounded by a characteristic wide gelatinous capsule.<br />
For descriptions of species, keys to taxa and additional information see Rippon (1982),<br />
Barnett et al. (1983), McGinnis (1980), Kurtzman and Fell (1988), Casadevall and Perfect<br />
(1988) and de Hoog et al. (2000).
Descriptions of Medical Fungi 51<br />
Cryptococcus albidus (Saito) Skinner<br />
Culture: Colonies (SDA) are cream-coloured smooth, mucoid glabrous yeast-like.<br />
Budding yeast cells only. No pseudohyphae present.<br />
Microscopy: Globose to ovoid budding yeast-like cells, 3.5-8.8 x 5.5-10.2 μm.<br />
India Ink Preparation: Positive - Distinct capsules are present.<br />
Physiological Tests: + Positive, - Negative, v Variable, w Weak, s Slow<br />
Germ Tube - L-Sorbose v L-Arabinose + D-Glucitol +<br />
Fermentation Sucrose + D-Arabinose v α-M-D-glucoside v<br />
Glucose - Maltose + D-Ribose v D-Gluconate +<br />
Galactose - Cellobiose + L-Rhamnose v DL-Lactate v<br />
Sucrose - Trehalose +,w D-Glucosamine - myo-Inositol +<br />
Maltose - Lactose v N-A-D-glucosamine - 2-K-D-gluconate +<br />
Lactose - Melibiose v Glycerol v D-Glucuronate +<br />
Trehalose - Raffinose + Erythritol v Nitrate +<br />
Assimilation Melezitose + Ribitol v Urease +<br />
Glucose + Soluble Starch v Galactitol v 0.1% Cycloheximide -<br />
Galactose v D-Xylose + D-Mannitol + Growth at 37 O C v<br />
C. albidus has variable growth at 37 O C, and rare human infections have been reported<br />
however its pathogenicity is questionable. RG-1 organism.<br />
Cryptococcus laurentii (Kufferath) Skinner<br />
Culture: Colonies (SDA) are cream-coloured, often becoming a deeper orange-yellow<br />
with age, with a smooth mucoid texture. Budding yeast cells only. No pseudohyphae<br />
present.<br />
Microscopy: Spherical and elongated budding yeast-like cells or blastoconidia, 2.0-<br />
5.5 x 3.0-7.0 μm. No pseudohyphae present.<br />
India Ink Preparation: Positive - Narrow but distinct capsules are present.<br />
Physiological Tests: + Positive, - Negative, v Variable, w Weak, s Slow<br />
Germ Tube - L-Sorbose v L-Arabinose + D-Glucitol +<br />
Fermentation Sucrose + D-Arabinose + α-M-D-glucoside +<br />
Glucose - Maltose + D-Ribose + D-Gluconate +<br />
Galactose - Cellobiose + L-Rhamnose + DL-Lactate v<br />
Sucrose - Trehalose + D-Glucosamine - myo-Inositol +<br />
Maltose - Lactose + N-A-D-glucosamine - 2-K-D-gluconate +<br />
Lactose - Melibiose + Glycerol v D-Glucuronate +<br />
Trehalose - Raffinose + Erythritol v Nitrate -<br />
Assimilation Melezitose + Ribitol + Urease +<br />
Glucose + Soluble Starch v Galactitol + 0.1% Cycloheximide -<br />
Galactose v D-Xylose + D-Mannitol + Growth at 37 O C -,w<br />
Note: some strains of C. laurentii may develop a brown pigment on Bird Seed agar and<br />
turn CGB media blue, similar to C. gattii, however C. laurentii assimilates both lactose<br />
and melibiose while C. gattii does not. Rare human infections have been reported<br />
however its pathogenicity is questionable. RG-1 organism.
52<br />
Descriptions of Medical Fungi<br />
Cryptococcus gattii (Vanbreus. & Takashio) Kwon-Chung & Boekhout<br />
Teleomorph: Filobasidiella bacillispora Kwon-Chung,<br />
Synonym: Cryptococcus neoformans var. gattii Vanbreus & Takashio<br />
Cryptococcus gattii has two serotypes (B and C) and has recently been reclassified as<br />
a separate species (Kwon-Chung et al. 2002). C. gattii generally has a more restricted<br />
geographical distribution than C. neoformans, causing human disease in climates<br />
ranging from temperate to tropical Australia, Papua New Guinea, parts of Africa, India,<br />
southeast Asia, Mexico, Brazil, Paraguay and Southern California, although recent<br />
infections have also been reported from Vancouver Island, Canada. Non-immunocompromised<br />
hosts are usually affected and large mass lesions in the lung and/or brain<br />
(cryptococcomas) are often present (Sorrell, 2001).<br />
Canavanine glycine bromothymol blue (CGB) agar (Kwon-Chung et al. 1982) is the<br />
media of choice to differentiate C. gattii from C. neoformans. This simple biotype test<br />
is based on the ability of C. gattii isolates to grow in the presence of L-canavanine and<br />
to assimilate glycine as a sole carbon source.<br />
C. gattii turns CGB agar blue within 2-5 days;<br />
C. neoformans does not grow on this medium<br />
Culture: Colonies (SDA) cream-coloured smooth, mucoid yeast-like colonies.<br />
Microscopy: Globose to ovoid budding yeast-like cells 3.0-7.0 x 3.3- 7.9 µm.<br />
India Ink Preparation: Positive - Distinct, wide gelatinous capsules are present.<br />
Dalmau Plate Culture on Cornmeal and Tween 80 Agar: Budding yeast cells only.<br />
No pseudohyphae present.<br />
Bird Seed Agar: Colonies turn dark brown in colour as they selectively absorb a<br />
brown pigment from this media. Colonies are often more mucoid when compared to<br />
C. neoformans (Staib, 1987).<br />
Canavanine-Glycine-Bromothymol Blue (CGB) Agar: turns blue within 2-5 days.<br />
Key Features: encapsulated yeast; absence of pseudohyphae; growth at 37 O C; positive<br />
hydrolysis of urea; negative fermentation of sugars and positive assimilation of<br />
glucose, maltose, sucrose, galactose, trehalose, raffinose, inositol, cellobiose, rhamnose,<br />
arabinose, melezitose and xylose, and negative assimilation of nitrate, lactose,<br />
melibiose, erythritol and soluble starch; growth on bird seed (Guizotia abyssinica seed)<br />
or caffeic acid agar - colonies turn a dark brown colour; growth on CGB agar turning it<br />
blue within 2-5 days. RG-2 organism, however mating experiments for the production<br />
of basidiospores should be done in an appropriate pathogen handling cabinet.
Descriptions of Medical Fungi 53<br />
Cryptococcus gattii (Vanbreus. & Takashio) Kwon-Chung & Boekhout<br />
Physiological Tests: + Positive, - Negative, v Variable, w Weak, s Slow<br />
Germ Tube - L-Sorbose v L-Arabinose +,w D-Glucitol +<br />
Fermentation Sucrose + D-Arabinose + α-M-D-glucoside +<br />
Glucose - Maltose + D-Ribose v D-Gluconate +<br />
Galactose - Cellobiose +,w L-Rhamnose + DL-Lactate -<br />
Sucrose - Trehalose + D-Glucosamine v myo-Inositol +<br />
Maltose - Lactose - N-A-D-glucosamine v 2-K-D-gluconate +<br />
Lactose - Melibiose - Glycerol - D-Glucuronate +<br />
Trehalose - Raffinose +,w Erythritol - Nitrate -<br />
Assimilation Melezitose + Ribitol v Urease +<br />
Glucose + Soluble Starch + Galactitol + 0.1% Cycloheximide -<br />
Galactose + D-Xylose + D-Mannitol + Growth at 37 O C +<br />
Antifungal<br />
MIC µg/mL<br />
MIC µg/mL<br />
Range MIC90 Antifungal Range MIC90 Fluconazole 1->64 16 Amphotericin B 0.03-2 0.25<br />
Itraconazole
54<br />
Descriptions of Medical Fungi<br />
Cryptococcus neoformans (Sanfelice) Vuillemin<br />
Culture: Colonies (SDA) cream-coloured smooth, mucoid yeast-like colonies.<br />
Microscopy: Globose to ovoid budding yeast-like cells 3.0-7.0 x 3.3- 7.9 µm.<br />
India Ink Preparation: Positive - Distinct, wide gelatinous capsules are present.<br />
Dalmau Plate Culture on Cornmeal and Tween 80 Agar: Budding yeast cells only.<br />
No pseudohyphae present.<br />
Bird Seed Agar: Colonies turn dark brown in colour as colonies selectively absorb a<br />
brown pigment from this media (Staib, 1987).<br />
Canavanine-Glycine-Bromothymol Blue (CGB) Agar: leaves this medium unchanged.<br />
Creatinine dextrose bromothymol blue thymine (CDBT) agar: Cryptococcus neoformans<br />
var. neoformans grows as bright red colonies, turning the medium a bright<br />
orange after 5 days. No colour change is observed for C. neoformans var. grubii.<br />
Physiological Tests: + Positive, - Negative, v Variable, w Weak, s Slow<br />
Germ Tube - L-Sorbose v L-Arabinose +,w D-Glucitol +<br />
Fermentation Sucrose + D-Arabinose + α-M-D-glucoside +<br />
Glucose - Maltose + D-Ribose v D-Gluconate +<br />
Galactose - Cellobiose +,w L-Rhamnose + DL-Lactate -<br />
Sucrose - Trehalose + D-Glucosamine v myo-Inositol +<br />
Maltose - Lactose - N-A-D-glucosamine v 2-K-D-gluconate +<br />
Lactose - Melibiose - Glycerol - D-Glucuronate +<br />
Trehalose - Raffinose +,w Erythritol - Nitrate -<br />
Assimilation Melezitose + Ribitol v Urease +<br />
Glucose + Soluble Starch + Galactitol + 0.1% Cycloheximide -<br />
Galactose + D-Xylose + D-Mannitol + Growth at 37 O C +<br />
Key Features: encapsulated yeast; absence of pseudohyphae; growth at 37 O C; positive<br />
hydrolysis of urea; negative fermentation of sugars and positive assimilation of<br />
glucose, maltose, sucrose, galactose, trehalose, raffinose, inositol, cellobiose, rhamnose,<br />
arabinose, melezitose and xylose, and negative assimilation of nitrate, lactose,<br />
melibiose, erythritol and soluble starch; growth on bird seed (Guizotia abyssinica seed)<br />
or caffeic acid agar - colonies turn a dark brown colour; does not growth on CGB agar<br />
(no colour change). RG-2 organism, however mating experiments for the production<br />
of basidiospores should be done in an appropriate pathogen handling cabinet.<br />
Antifungal<br />
MIC µg/mL<br />
MIC µg/mL<br />
Range MIC90 Antifungal Range MIC90 Fluconazole 1->64 8 Amphotericin B 0.03-2 0.5<br />
Itraconazole
Descriptions of Medical Fungi 55<br />
Cunninghamella bertholletiae Stadel<br />
Synonyms: Cunninghamella elegans Lendner<br />
Cunninghamella echinulata var. elegans (Lendner) Lunn & Shipton<br />
The genus Cunninghamella is characterised by white to grey, rapidly growing colonies,<br />
producing erect, straight, branching sporangiophores. These sporangiosphores<br />
end in globose or pyriform-shaped vesicles from which several one-celled, globose to<br />
ovoid, echinulate or smooth-walled sporangiola develop on swollen denticles. Chlamydospores<br />
and zygospores may also be present.<br />
Colonies are very fast growing, white at first, but becoming rather dark grey and powdery<br />
with sporangiola development. Sporangiophores to 20 μm wide, straight, with<br />
verticillate or solitary branches. Vesicles subglobose to pyriform, the terminal ones up<br />
to 40 µm and the lateral ones 10-30 µm in diameter. Sporangiola are globose (7-11<br />
µm diameter), or ellipsoidal (9-13 x 6-10 μm), verrucose or short-echinulate, hyaline<br />
singly but brownish in mass. Temperature: optimum 25 to 30 O C: maximum up to 50 O C.<br />
RG-2 organism.<br />
Cunninghamella species are mainly soil fungi of the Mediterranean and subtropical<br />
zones; they are only rarely isolated in temperate regions. The genus now contains<br />
seven species with C. bertholletiae the only known species to cause disease in man<br />
and animals which is often associated with trauma and immunosuppression.<br />
Key Features: zygomycete, clinical isolates grow at 40 O C, one-celled, globose to<br />
ovoid, echinulate sporangiola borne on swollen terminal or lateral globose to clavate<br />
fertile vesicles.<br />
Once again, there has been some confusion as to the correct name of this zygomycete.<br />
Many medical mycologists (McGinnis, 1980, Weitzman, 1984, and Rippon, 1988)<br />
preferred the name Cunninghamella bertholletiae because of the thermophilic nature<br />
of human isolates that grow at temperatures as high as 45 O C. However, Samson<br />
(1969) and Domsch et al. (1980) preferred the name Cunninghamella elegans and<br />
Lunn and Shipton (1983) went further and reduced C. elegans (= C. bertholletiae) to<br />
a variety of Cunninghamella echinulata; i.e. C. echinulata var. elegans. However, C.<br />
bertholletiae is currently the most acceptable name; C. elegans differs by having purely<br />
grey colonies and by not growing at temperatures above 40 O C (Weitzman and Crist,<br />
1979 and de Hoog et al. 2000).<br />
Antifungal<br />
MIC µg/mL<br />
MIC µg/mL<br />
Antifungal<br />
Range MIC Range MIC 90 90<br />
Fluconazole >64 >64 Amphotericin B 0.125-8 2<br />
Itraconazole 0.125-4 2 Flucytosine >256 >256<br />
Posaconazole 0.003-1 1 Voriconazole 8->64 >64<br />
Very limited data, antifungal susceptibility testing of individual strains is recommended.<br />
Sun et al. (2002), Dannaoui et al. (2003), Espinel-Ingroff (2001, 2003), Singh et al.<br />
(2005), Sabatelli et al. (2006) and WCH in-house data.
56<br />
Descriptions of Medical Fungi<br />
10 μm<br />
Cunninghamella bertholletiae Stadel<br />
10 μm<br />
Microscopic morphology of Cunninghamella bertholletiae showing simple sporangiophores<br />
forming a swollen, terminal vesicle around which single-celled, globose<br />
to ovoid sporangiola develop on swollen denticles.<br />
For descriptions of species, keys to taxa and additional information see McGinnis<br />
(1980), Weitzman (1984), Lunn and Shipton (1983), Domsch et al. (1980), Samson<br />
(1969), de Hoog et al (2000) and Ellis (2005b).
Descriptions of Medical Fungi 57<br />
Teleomorph: Cochliobolus Drechsler<br />
Curvularia Boedijn<br />
Colonies are fast growing, suede-like to downy, brown to blackish brown with a black<br />
reverse. Conidia are pale brown, with three or more transverse septa (phragmoconidia)<br />
and are formed apically through a pore (poroconidia) in a sympodially elongating<br />
geniculate conidiophore similar to Drechslera. Conidia are cylindrical or slightly<br />
curved, with one of the central cells being larger and darker, germination is bipolar and<br />
some species may have a prominent hilum.<br />
The genus Curvularia contains some 35 species which are mostly subtropical and<br />
tropical plant parasites; however three ubiquitous species, C. lunata, C. pallescens<br />
and C. geniculata have been recovered from human infections, principally from cases<br />
of mycotic keratitis. However, cases of subcutaneous, sinusitis, endocarditis, peritonitis<br />
and disseminated infection have also been reported in immunosuppressed patients.<br />
RG-1 organisms.<br />
Key Features: dematiaceous hyphomycete producing sympodial, pale brown,<br />
cylindrical or slightly curved phragmoconidia, with one of the central cells being larger<br />
and darker.<br />
For descriptions of species, keys to taxa and additional information see Ellis (1971),<br />
Domsch et al. (1980), McGinnis (1980), Rippon (1988) and de Hoog et al. (2000).<br />
Antifungal<br />
20 µm<br />
Conidia of Curvularia lunata.<br />
MIC µg/mL MIC µg/mL MIC µg/mL<br />
Antifungal Antifungal<br />
Range Range Range<br />
Amphotericin B 0.03-16 Itraconazole 0.03-32 Voriconazole 0.06-1<br />
Very limited data, antifungal susceptibility testing of individual strains is recommended.<br />
McGinnis and Pasarell (1998), Espinel-Ingroff et al. (2001) and WCH in-house data.
58<br />
Descriptions of Medical Fungi<br />
Teleomorph: Nectria (Fries) Fr.<br />
Cylindrocarpon Wollenw.<br />
Colonies are fast growing, hyaline or bright-coloured, suede-like or woolly. Sporodochia<br />
may occasionally be present. Conidiophores consist of simple or repeatedly verticillate<br />
phialides, arranged in brush-like structures. Phialides are cylindrical to subulate,<br />
with small collarettes producing hyaline, smooth-walled conidia, which are arranged in<br />
slimy masses. Two types of conidia may be produced; macroconidia which are one to<br />
several septate, hyaline, straight or curved, cylindrical to fusiform, with a rounded apex<br />
and flat base; and microconidia which are one-celled, which are usually clearly distinct<br />
from the macroconidia. Chlamydospores may be present or absent, hyaline to brown,<br />
spherical, formed singly, in chains or in clumps, intercalary or terminal. RG-2 organism<br />
if isolated from humans.<br />
The genus contains 35 species, is widespread, isolated mostly from soil and is recorded<br />
as an occasional human and animal pathogen. Cylindrocarpon differs from<br />
Fusarium by lacking an asymmetrical foot-cell on the macroconidia.<br />
For descriptions of species, keys to taxa and additional information see Booth (1966),<br />
Domsch et al. (1980) and de Hoog et al. (2000).<br />
15 µm<br />
15 µm<br />
Culture, chlamydospores and macroconidia of Cylindrocarpon lichenicola.
Descriptions of Medical Fungi 59<br />
Teleomorph: Pyrenophora Fries<br />
Drechslera Ito<br />
Colonies are fast growing, suede-like to downy, brown to blackish brown with a black<br />
reverse. Conidia are pale to dark brown, usually cylindrical or subcylindrical, straight,<br />
smooth-walled, and are formed apically through a pore (poroconidia) on a sympodially<br />
elongating, geniculate conidiophore. Conidia are transversely septate (phragmoconidia),<br />
with the septum delimiting the basal cell formed first during conidium maturation.<br />
Germinating is from any or all cells and the hilum is not protuberant. RG-1 organism.<br />
McGinnis et al. (1986b) have reviewed the isolates from human and animal disease<br />
purported to be Drechslera or Helminthosporium and concluded that all pathogenic<br />
isolates examined actually belong to the genera Bipolaris or Exserohilum.<br />
Key Features: dematiaceous hyphomycete producing sympodial, pale brown,<br />
cylindrical or subcylindrical, transversely septate poroconidia.<br />
For descriptions of species, keys to taxa and additional information see Luttrell (1978),<br />
Ellis (1971 and 1976), Domsch et al. (1980), McGinnis (1980), McGinnis et al. (1986b),<br />
Sivanesan (1987), Rippon (1988) and de Hoog et al. (2000). Also see Descriptions for<br />
Bipolaris, Curvularia and Exserohilum.<br />
Antifungal<br />
Conidia of Drechslera.<br />
20 µm<br />
MIC µg/mL MIC µg/mL MIC µg/mL<br />
Antifungal Antifungal<br />
Range Range Range<br />
Amphotericin B 0.25 Itraconazole 0.25 Voriconazole 0.06<br />
Very limited data, antifungal susceptibility testing of individual strains is recommended.<br />
McGinnis and Pasarell (1998).
60<br />
Descriptions of Medical Fungi<br />
Epicoccum purpurascens Ehrenb. ex Schlecht.<br />
Synonym: Epicoccum nigrum Link<br />
Colonies are fast growing, suede-like to downy, with a strong yellow to orange-brown<br />
diffusible pigment. When sporulating numerous black sporodochia (aggregates of<br />
conidiophores) are visible. Conidia are formed singly on densely compacted, nonspecialised,<br />
determinant, slightly pigmented conidiophores. Conidia are globose to<br />
pyriform, mostly l5-25 µm diameter with a funnel-shaped base and broad attachment<br />
scar, often seceding with a protuberant basal cell; i.e. aleuric or rhexolytic dehiscence<br />
of conidia. Conidia become multicellular (dictyoconidia), darkly pigmented and have a<br />
verrucose external surface. RG-1 organism.<br />
Epicoccum purpurascens is a cosmopolitan saprophyte of world-wide distribution which<br />
is occasionally isolated as a contaminant from clinical specimens like skin.<br />
Key Features: dematiaceous hyphomycete producing darkly pigmented, large globose<br />
to pyriform, verrucose dictyoconidia on a sporodochium.<br />
For descriptions of species, keys to taxa and additional information see Ellis (1971),<br />
Domsch et al. (1980), McGinnis (1980) and Samson et al. (1995).<br />
15 µm<br />
Conidia of Epicoccum purpurascens.
Descriptions of Medical Fungi 61<br />
Epidermophyton floccosum (Harz) Langeron et Milochevitch<br />
Colonies (SDA) are usually slow growing, greenish-brown or khaki-coloured with a<br />
suede-like surface, raised and folded in the centre, with a flat periphery and submerged<br />
fringe of growth. Older cultures may develop white pleomorphic tufts of mycelium. A<br />
deep yellowish-brown reverse pigment is usually present. Microscopic morphology<br />
shows characteristic smooth, thin-walled macroconidia which are often produced in<br />
clusters growing directly from the hyphae. Numerous chlamydospores are formed in<br />
older cultures. Microconidia are not formed.<br />
Epidermophyton floccosum is an anthropophilic dermatophyte with a world-wide distribution<br />
which often causes tinea pedis, tinea cruris, tinea corporis and onychomycosis.<br />
It is not known to invade hair in vivo and no specific growth requirements have been<br />
reported. RG-2 organism.<br />
Key Features: culture characteristics, microscopic morphology and clinical disease.<br />
For descriptions of species, keys to taxa and additional information see Rebell and<br />
Taplin (1970), Mackenzie et al. (1987), Rippon (1988) and de Hoog et al. (2000).<br />
20 µm<br />
15 µm<br />
Culture, macroconidia and chlamydospores of E. floccosum.<br />
Antifungal<br />
MIC µg/mL<br />
Range MIC90 Antifungal<br />
MIC µg/mL<br />
Range MIC90 Griseofulvin 0.06-2 1 Amphotericin B 0.03-0.5 0.25<br />
Itraconazole 0.01-8 0.125 Fluconazole 0.5->64 >64<br />
Terbinafine 0.01-1 0.06 Voriconazole 0.01-8 0.125<br />
Fernandez-Torres et al. (2001) and Sabatelli et al. (2006) and WCH in-house data.
62<br />
Descriptions of Medical Fungi<br />
Exophiala dermatitidis (Kano) de Hoog<br />
Synonym: Wangiella dermatitidis (Kano) McGinnis<br />
Colonies are slow growing, initially yeast-like and black, becoming suede-like, olivaceous<br />
grey with the development of aerial mycelium with age. The initial yeast-like<br />
phase is referred to as the Phaeococcomyces exophialae synanamorph, which is characterised<br />
by unicellular, ovoid to elliptical, budding yeast-like cells. The yeast-like cells<br />
are hyaline and thin-walled when young becoming darkly pigmented (dematiaceous)<br />
and thick-walled when mature. With the development of mycelium, flask-shaped to cylindrical<br />
annellides are produced. Conidia are hyaline to pale brown, one-celled, round<br />
to obovoid, 2.0-4.0 x 2.5-6.0 µm, smooth-walled and accumulate in slimy balls at the<br />
apices of the annellides or down their sides. Cultures grow at 42 O C.<br />
E. dermatitidis has been isolated from plant debris and soil and is a recognised causative<br />
agent of mycetoma and phaeohyphomycosis in humans. RG-2 organism.<br />
For descriptions of species, keys to taxa and additional information see de Hoog and<br />
Hermanides-Nijhof (1977), McGinnis (1980), Hohl et al. (1983), Nishimura and Miyaji<br />
(1983), Matsumoto et al. (1984), Dixon and Polak-Wyss (1991), de Hoog et al.<br />
(2000).<br />
Antifungal<br />
10 µm<br />
Annellides and conidia of Exophiala dermatitidis.<br />
MIC µg/mL<br />
MIC µg/mL<br />
Range MIC90 Antifungal<br />
Range MIC90 Itraconazole 0.03-2 0.5 Amphotericin B 0.03-2 0.5<br />
Voriconazole 0.06-0.5 0.25 Posaconazole 0.03-1 nd<br />
Limited data, antifungal susceptibility testing of individual strains is recommended.<br />
McGinnis and Pasarell (1998), Espinel-Ingroff (2001), Espinel-Ingroff et al. (2001),<br />
Pfaller et al. (2002a) and WCH in-house data (nd = not done).
Descriptions of Medical Fungi 63<br />
Exophiala jeanselmei Complex<br />
Synonyms: Phialophora jeanselmei (Langeron) Emmons<br />
E. jeanselmei has long been recognised as heterogeneous (de Hoog 1977). Recent<br />
molecular studies have redefined Exophiala jeanselmei and three additional species<br />
have been identified: E. oligosperma, E. nishimurae, and E. xenobiotica (Vitale and<br />
de Hoog, 2002 , de Hoog et al. 2003, 2006). These species are morphologically very<br />
similar and can best be distinguished by genetic analysis.<br />
Conidiogenous cells are predominantly annellidic and erect, multicellular conidiophores<br />
are absent. No growth at 40 O C.<br />
E. jeanselmei Mature conidiogenous cells rocket-shaped, slightly darker than<br />
the supporting hyphae, with regular tapering annellated zones.<br />
E. oligosperma Mature conidiogenous cells remain concolorous with supporting<br />
hyphae and may be intercalary and lateral, the latter being flask<br />
or rocket-shaped. Annellated zones have the appearance of inconspicuous<br />
flat scars. Chlamydospores are absent.<br />
E. nishimurae Similar morphology to E. oligosperma, however large chlamydospore-like<br />
cells are present.<br />
E. xenobiotica A segregant genotype of the E. jeanselmei complex with less<br />
melanised conidiogenous cells.<br />
Colonies are initially smooth, greenish-grey to black, mucoid and yeast-like, becoming<br />
raised and developing tufts of aerial mycelium with age, often becoming domeshaped<br />
and suede-like in texture. Reverse is olivaceous-black. Numerous ellipsoidal,<br />
yeast-like, budding cells are usually present, especially in young cultures. Scattered<br />
amongst these yeast-like cells are larger, inflated, subglobose to broadly ellipsoidal<br />
cells (germinating cells) which give rise to short torulose hyphae that gradually change<br />
into unswollen hyphae. Conidia are formed on lateral pegs either arising apically or laterally<br />
at right or acute angles from essentially undifferentiated hyphae or from strongly<br />
inflated detached conidia. Conidiogenous pegs are 1-3 µm long, slightly tapering and<br />
imperceptibly annellate. Conidia are hyaline, smooth, thin-walled, broadly ellipsoidal,<br />
3.2-4.4 x 1.2-2.2 µm, and with inconspicuous basal scars. Cultures grow at 37 O C but<br />
not at 40 O C. RG-2 organism.<br />
E. jeanselmei has a world-wide distribution and is a recognised causative agent of<br />
mycetoma and phaeohyphomycosis in humans.<br />
For descriptions of species, keys to taxa and additional information see de Hoog and<br />
Hermanides-Nijhof (1977), de Hoog (1977, 1985), McGinnis and Padhye (1977),<br />
McGinnis (1978, 1980), Domsch et al. (1980), Nishimura and Miyaji (1983), Matsumoto<br />
et al. (1987), Dixon and Polak-Wyss (1991) and de Hoog et al. (2000, 2003, 2006).<br />
Antifungal<br />
MIC µg/mL<br />
MIC µg/mL<br />
Range MIC90 Antifungal<br />
Range MIC90 Itraconazole 0.03-2 0.5 Amphotericin B 0.03-4 0.5<br />
Voriconazole 0.06-2 0.5 Posaconazole 0.25-0.5 0.5<br />
Limited data, antifungal susceptibility testing of individual strains is recommended.<br />
McGinnis and Pasarell (1998), Espinel-Ingroff et al. (2001), Nucci et al. (2001) and<br />
WCH in-house data.
64<br />
Descriptions of Medical Fungi<br />
Exophiala jeanselmei/spinifera Complex<br />
5 µm<br />
15 µm<br />
5 µm<br />
Annellides, conidia and conidiogenous pegs (annellides) on yeast-like cells and<br />
torulose hyphae of Exophiala jeanselmei.<br />
10 µm<br />
Erect, multiseptate conidiophores that are darker than the supporting hyphae,<br />
with long annellated zones and conidia of Exophiala spinifera.
Descriptions of Medical Fungi 65<br />
Exophiala spinifera Complex<br />
Synonyms: Phialophora spinifera Nielsen & Conant<br />
Rhinocladiella spinifera (Nielsen & Conant) de Hoog<br />
Recent molecular studies have re-examined Exophiala spinifera and have recognised<br />
two species: E. spinifera and E. attenuata (Vitale and de Hoog, 2002). These two<br />
species are morphologically very similar and can best be distinguished by genetic<br />
analysis.<br />
Conidiogenous cells are predominately annellidic and erect, multicellular conidiophores<br />
that are darker than the supporting hyphae are present. No growth at 40 O C.<br />
E. spinifera Annellated zones are long with clearly visible, frilled annellations.<br />
E. attenuata Annellated zones are inconspicuous and degenerate.<br />
Colonies are initially mucoid and yeast-like, black, becoming raised and developing<br />
tufts of aerial mycelium with age, finally becoming suede-like to downy in texture. Reverse<br />
is olivaceous-black. Conidiophores are simple or branched, erect or sub-erect,<br />
spine-like with rather thick brown pigmented walls. Conidia are formed in basipetal succession<br />
on lateral pegs either arising apically or laterally at right or acute angles from<br />
the spine-like conidiophores or from undifferentiated hyphae. Conidiogenous pegs<br />
are 1-3 µm long, slightly tapering and imperceptibly annellate. Conidia are one-celled,<br />
subhyaline, smooth, thin-walled, subglobose to ellipsoidal, 1.0-2.9 x 1.8-2.5 µm, and<br />
aggregate in clusters at the tip of each annellide. Toruloid hyphae and yeast-like cells<br />
with secondary conidia are typically present. No growth at 40 O C. RG-2 organism.<br />
E. spinifera has a world-wide distribution and is a recognised causative agent of<br />
mycetoma and phaeohyphomycosis in humans.<br />
For descriptions of species, keys to taxa and additional information see de Hoog and<br />
Hermanides-Nijhof (1977), McGinnis and Padhye (1977), Domsch et al. (1980), McGinnis<br />
(1980), Nishimura and Miyaji (1983), de Hoog (1985), Matsumoto et al. (1987),<br />
Dixon and Polak-Wyss (1991) and de Hoog et al. (2000, 2003, 2006).<br />
Antifungal<br />
MIC µg/mL MIC µg/mL MIC µg/mL<br />
Antifungal Antifungal<br />
Range Range Range<br />
Amphotericin B 0.125-1 Itraconazole 0.03-1 Voriconazole 0.125-1<br />
Very limited data, antifungal susceptibility testing of individual strains is recommended.<br />
McGinnis and Pasarell (1998), Espinel-Ingroff et al. (2001) and WCH in-house data.
66<br />
Descriptions of Medical Fungi<br />
Exserohilum Leonard and Suggs<br />
Colonies are grey to blackish-brown, suede-like to floccose in texture and have an olivaceous<br />
black reverse. Conidia are straight, curved or slightly bent, ellipsoidal to fusiform<br />
and are formed apically through a pore (poroconidia) on a sympodially elongating<br />
geniculate conidiophore. Conidia have a strongly protruding, truncate hilum and the<br />
septum above the hilum is usually thickened and dark, with the end cells often paler<br />
than other cells, walls often finely roughed. Conidial germination is bipolar.<br />
The genus Exserohilum may be differentiated from the closely related genera Bipolaris<br />
and Dreschlera by forming conidia with a strongly protruding truncate hilum (i.e.<br />
exserted hilum). The hilum is defined as “a scar on a conidium at the point of attachment<br />
to the conidiophore”. In Drechslera species, the hilum does not protrude; in Bipolaris<br />
species the hilum protrudes only slightly. Several species of Exserohilum have<br />
been reported as agents of phaeohyphomycosis, notably E. rostratum (= E. halodes),<br />
E. mcginnisii and E. longirostratum. RG-1 organisms.<br />
Key Features: dematiaceous hyphomycete producing sympodial, transverse septate,<br />
ellipsoidal to fusiform conidia with a strongly protruding, truncate hilum.<br />
For descriptions of species, keys to taxa and additional information see Domsch et<br />
al. (1980), Alcorn (1983), Adam et al. (1986), McGinnis et al. (1986b), Rippon (1988),<br />
Burges et al. (1987), Dixon and Polak-Wyss (1991) and de Hoog et al. (2000).<br />
Antifungal<br />
20 µm<br />
20 µm<br />
Conidiophores and conidia with distinctive hilum (arrow) of E. rostratum.<br />
MIC µg/mL MIC µg/mL MIC µg/mL<br />
Antifungal Antifungal<br />
Range Range Range<br />
Amphotericin B 0.125-2 Itraconazole 0.03-0.5 Voriconazole 0.03-0.5<br />
Very limited data, antifungal susceptibility testing of individual strains is recommended.<br />
McGinnis and Pasarell (1998) and WCH in-house data.
Descriptions of Medical Fungi 67<br />
Fonsecaea pedrosoi/monophora Complex<br />
Morphologically the genus Fonsecaea is defined by the presence of indistinct melanised<br />
conidiophores with blunt, scattered denticles bearing conidia singly or in short<br />
chains that eventually become branched. de Hoog et al. (2004) revised the genus on<br />
the basis of ribosomal DNA internal transcribed spacer (ITS) sequence data recognising<br />
two species; F. pedrosoi and F. monophora. The previously described species F.<br />
compacta was found to be a morphological variant of F. pedrosoi. Morphological F.<br />
pedrosoi and F. monophora are very similar and can best be distinguished by genetic<br />
analysis. F. monophora on average has slightly longer conidial chains and slightly<br />
shorter denticles than F. pedrosoi. All strains grow at 37 O C but not at 40 O C. Both species<br />
are recognised etiologic agents of chromoblastomycosis. RG-2 organism.<br />
Colonies are slow growing, flat to heaped and folded, suede-like to downy, olivaceous<br />
to black with black reverse. Conidiogenous cells pale olivaceous, arranged in loosely<br />
branched systems, with prominent denticles. Conidia pale olivaceous, clavate to<br />
ellipsoidal, in short chains, subhyaline, smooth and thin-walled, 3.5-5 x 1.5-2 µm.<br />
For descriptions of species, keys to taxa and additional information see McGinnis<br />
(1980), Dixon and Polak-Wyss (1991), de Hoog et al. (2000), de Hoog et al. (2004).<br />
Antifungal<br />
Conidiophores and conidia of Fonsecaea.<br />
10 µm<br />
MIC µg/mL<br />
MIC µg/mL<br />
Range MIC90 Antifungal<br />
Range MIC90 Itraconazole 0.03-1 0.25 Amphotericin B 0.03-2 1<br />
Voriconazole 0.06-1 0.06 Posaconazole 0.06-1 nd<br />
Limited data, antifungal susceptibility testing of individual strains is recommended.<br />
McGinnis and Pasarell (1998), Espinel-Ingroff et al. (2001), Espinel-Ingroff (2003)<br />
and WCH in-house data (nd = not done).
68<br />
Descriptions of Medical Fungi<br />
Fusarium Link ex Fries<br />
Colonies are usually fast growing, pale or bright coloured (depending on the species)<br />
with or without a cottony aerial mycelium. The colour of the thallus varies from whitish<br />
to yellow, pink, red or purple shades. Species of Fusarium typically produce both macro-<br />
and microconidia from slender phialides. Macroconidia are hyaline, two- to severalcelled,<br />
fusiform to sickle-shaped, mostly with an elongated apical cell and pedicellate<br />
basal cell. Microconidia are one- or two-celled, hyaline, smaller than macroconidia,<br />
pyriform, fusiform to ovoid, straight or curved. Chlamydospores may be present or<br />
absent.<br />
Cultures of F. oxysporum showing purple pigmentation<br />
and F. subglutinans showing pink pigmentation.<br />
Identification of Fusarium species is often difficult due to the variability between isolates<br />
(e.g. in shape and size of conidia and colony colour) and because not all features<br />
required are always well developed (e.g. the absence of macroconidia in some isolates<br />
after subculture). The important characters used in the identification of Fusarium species<br />
are as follows. Note: sporulation may need to be induced in some isolates and a<br />
good slide culture is essential.<br />
1. Colony growth diameters on potato dextrose agar and/or potato sucrose agar after<br />
incubation in the dark for 4 days at 25 O C.<br />
2. Culture pigmentation on potato dextrose agar and/or potato sucrose agar after incubation<br />
for 10-14 days with daily exposure to light.<br />
3. Microscopic morphology including shape of the macroconidia; presence or absence<br />
of microconidia; shape and mode of formation of microconidia; nature of the conidiogenous<br />
cell bearing microconidia; and presence or absence of chlamydospores.<br />
Most Fusarium species are soil fungi and have a world-wide distribution. Some are<br />
plant pathogens, causing root and stem rot, vascular wilt or fruit rot. Several species,<br />
notably F. oxysporum, F. solani and F. moniliforme are recognised as being pathogenic<br />
to man and animals causing hyalohyphomycosis (especially in burn victims and<br />
bone marrow transplant patients), mycotic keratitis and onychomycosis. Other species<br />
cause storage rot and are important mycotoxin producers.<br />
For descriptions of species, keys to taxa and additional information see Booth (1971<br />
and 1977), Domsch et al. (1980), McGinnis (1980), Burgess and Liddell (1983), Rippon<br />
(1988), Samson et al. (1995) and de Hoog et al. (2000).
Descriptions of Medical Fungi 69<br />
15 µm<br />
Fusarium oxysporum Schlecht<br />
Colonies growing rapidly, 4.5 cm in 4 days, aerial mycelium white, becoming purple,<br />
with discrete orange sporodochia present in some strains; reverse hyaline to dark blue<br />
or dark purple. Conidiophores are short, single, lateral monophialides in the aerial<br />
mycelium, later arranged in densely branched clusters. Macroconidia are fusiform,<br />
slightly curved, pointed at the tip, mostly three septate, basal cells pedicellate, 23-54 x<br />
3-4.5 µm. Microconidia are abundant, never in chains, mostly non-septate, ellipsoidal<br />
to cylindrical, straight or often curved, 5-12 x 2.3 - 3.5 µm. Chlamydospores are terminal<br />
or intercalary, hyaline, smooth or rough-walled, 5-13 µm. In contrast to F. solani<br />
the phialides are short and mostly non-septate. RG-2 organism.<br />
Antifungal<br />
15 µm<br />
Microconidia on short phialides and macroconidia of F. oxysporum.<br />
MIC µg/mL<br />
MIC µg/mL<br />
Range MIC<br />
Antifungal<br />
Range MIC 90 90<br />
Itraconazole 0.5->16 >8 Amphotericin B 0.25->16 1-2<br />
Voriconazole 0.25->8 1-2 Posaconazole 1->8 4<br />
Limited data, antifungal susceptibility testing of individual strains is recommended.<br />
Espinel-Ingroff et al. (2001), Espinel-Ingroff (2001, 2003), Diekema et al. (2003),<br />
Cuenca-Estrella et al. (2006), Sabatelli et al. (2006) and WCH in-house data.
70<br />
Descriptions of Medical Fungi<br />
Fusarium solani (Mart.) Sacc.<br />
Colonies growing rapidly, 4.5 cm in 4 days, aerial mycelium white to cream, becoming<br />
bluish-brown when sporodochia are present. Macroconidia are formed after 4-7 days<br />
from short multi-branched conidiophores which may form sporodochia. They are 3- to<br />
5- septate (usually 3- septate), fusiform, cylindrical, often moderately curved, with an<br />
indistinctly pedicellate foot cell and a short blunt apical cell, 28-42 x 4-6 µm. Microconidia<br />
are usually abundant, cylindrical to oval, one- to two-celled and formed from long<br />
lateral phialides, 8-16 x 2-4.5 µm. Chlamydospores are hyaline, globose, smooth to<br />
rough-walled, borne singly or in pairs on short lateral hyphal branches or intercalary,<br />
6-10 µm. RG-2 organism.<br />
Antifungal<br />
15 µm<br />
15 µm<br />
15 µm<br />
Microconidia on long phialides, macroconidia and chlamydospores of F. solani.<br />
MIC µg/mL<br />
MIC µg/mL<br />
Range MIC<br />
Antifungal<br />
Range MIC 90 90<br />
Itraconazole 0.25->16 >8 Amphotericin B 0.25->16 4<br />
Voriconazole 0.125->8 4 (>8) Posaconazole >8 >8<br />
Limited data, antifungal susceptibility testing of individual strains is recommended.<br />
Espinel-Ingroff et al. (2001), Espinel-Ingroff (2001, 2003), Diekema et al. (2003),<br />
Cuenca-Estrella et al. (2006), Sabatelli et al. (2006) and WCH in-house data.
Descriptions of Medical Fungi 71<br />
Geotrichum Link<br />
Species of the genus Geotrichum typically produce chains of hyaline, smooth, onecelled,<br />
subglobose to cylindrical arthroconidia by the holoarthric fragmentation of undifferentiated<br />
hyphae. Conidia may also develop sympodially and chlamydospores and<br />
endoconidia may also be present. The arthroconidia, which are quite variable in size<br />
may germinate at one end giving the appearance of a bud. However, the latter develops<br />
into a septate mycelium. True blastoconidia production is not found in the genus.<br />
This characteristic distinguishes the genus Geotrichum from Trichosporon which usually<br />
does produce blastoconidia.<br />
The need to exercise care when identifying species of Geotrichum must be stressed,<br />
as this name has often been used erroneously to describe any hyaline hyphomycete<br />
producing arthroconidia (McGinnis, 1980). Geotrichum species may be differentiated<br />
from each other using physiological and biochemical tests similar to those used for the<br />
identification of yeasts (Gueho, 1979 and Buchta and Otcenasek, 1988).<br />
For descriptions of species, keys to taxa and additional information see Gueho (1979),<br />
Domsch et al. (1980), McGinnis (1980), Barnett et al. (1983), Buchta and Otcenasek<br />
(1988), Samson et al. (1995), Kurtzman and Fell (1998) and de Hoog et al. (2000).<br />
Arthroconidium formation in G. candidum. Hyphal elements are progressively<br />
compartmentalised by fragmentation of septa. Conidial secession is<br />
by the centripetal separation (schizolysis) of a so called double septum and<br />
concomitant rupture of the original outer hyphal wall layer.<br />
Antifungal<br />
15 µm<br />
15 µm<br />
MIC µg/mL<br />
MIC µg/mL<br />
Range MIC90 Antifungal Range MIC90 Fluconazole 0.25-32 8-32 Amphotericin B 0.06-1.0 0.125<br />
Itraconazole 0.03->32 >32 Flucytosine 0.125-16 4<br />
Voriconazole 0.03-0.5 0.25<br />
Limited data, antifungal susceptibility testing of individual strains is recommended.<br />
Girmenia et al. (2003), Kucukates et al. (2005) and WCH in-house data.
72<br />
Descriptions of Medical Fungi<br />
Geotrichum candidum Link<br />
Teleomorph: Galactomyces geotrichum (Butler & Petersen) Redhead & Malloch<br />
Colonies are fast growing, flat, white to cream, dry and finely suede-like with no reverse<br />
pigment. Hyphae are hyaline, septate, branched and break up into chains of hyaline,<br />
smooth, one-celled, subglobose to cylindrical arthroconidia. They are 6-12 x 3-6 µm in<br />
size and are released by the separation of a double septum. RG-1 organism.<br />
Physiological Tests: + Positive, - Negative, v Variable, w Weak, s Slow, n No data<br />
Germ Tube - L-Sorbose + L-Arabinose - D-Glucitol +<br />
Fermentation Sucrose - D-Arabinose - α-M-D-glucoside -<br />
Glucose v Maltose - D-Ribose v D-Gluconate -<br />
Galactose v Cellobiose - L-Rhamnose - DL-Lactate v<br />
Sucrose - Trehalose + D-Glucosamine - myo-Inositol -<br />
Maltose - Lactose - N-A-D-glucosamine n 2-K-D-gluconate -<br />
Lactose - Melibiose - Glycerol + D-Glucuronate -<br />
Trehalose - Raffinose - Erythritol - Nitrate -<br />
Assimilation Melezitose - Ribitol v Urease -<br />
Glucose + Soluble Starch - Galactitol - 0.1% Cycloheximide +<br />
Galactose + D-Xylose + D-Mannitol v Growth at 37 O C v<br />
Geotrichum candidum is an extremely common fungus with a world-wide distribution.<br />
Pulmonary involvement is the most frequently reported form of the disease, but bronchial,<br />
oral, vaginal, cutaneous and alimentary infections have also been noted.<br />
Geotrichum capitatum (Diddens & Lodder) v. Arx<br />
Teleomorph: Dipodascus capitatis de Hoog et al.<br />
Synonyms: Trichosporon capitatum, Blastoschizomyces capitis<br />
Colonies are moderately fast growing, flat, whitish, and finely suede-like with no reverse<br />
pigment. Hyphae are profusely branched at acute angles, with terminal and intercalary<br />
conidiogenous cells which form long, cicatrized rachids on which conidia are borne.<br />
Conidia are hyaline, smooth, one-celled, cylindrical to clavate, with a rounded apex<br />
and flat base, 7-10 x 2.5-3.5 µm. Rectangular arthroconidia are also often present.<br />
RG-2 organism.<br />
Physiological Tests: + Positive, - Negative, v Variable, w Weak, s Slow, n No data<br />
Germ Tube - L-Sorbose v L-Arabinose - D-Glucitol -<br />
Fermentation Sucrose - D-Arabinose - α-M-D-glucoside -<br />
Glucose - Maltose - D-Ribose v D-Gluconate -<br />
Galactose - Cellobiose - L-Rhamnose - DL-Lactate +<br />
Sucrose - Trehalose - D-Glucosamine - myo-Inositol -<br />
Maltose - Lactose - N-A-D-glucosamine n 2-K-D-gluconate -<br />
Lactose - Melibiose - Glycerol + D-Glucuronate -<br />
Trehalose - Raffinose - Erythritol - Nitrate -<br />
Assimilation Melezitose - Ribitol - Urease -<br />
Glucose + Soluble Starch - Galactitol - 0.1% Cycloheximide +<br />
Galactose + D-Xylose - D-Mannitol - Growth at 40 O C +<br />
Geotrichum capitatum occurs quite commonly in humans, usually as a transient component<br />
of normal skin flora and sputum. Systemic infections including pulmonary,<br />
fungemia and endocarditis have been reported in immunosuppressed patients.
Descriptions of Medical Fungi 73<br />
Gliocladium Corda<br />
The genus Gliocladium is often described as a counterpart of Penicillium with slimy<br />
conidia. Colonies are fast growing, suede-like to downy in texture, white at first, sometimes<br />
pink to salmon, becoming pale to dark green with sporulation. The most characteristic<br />
feature of the genus is the distinctive erect, often densely penicillate conidiophores<br />
with phialides which bear slimy, one-celled hyaline to green, smooth-walled<br />
conidia in heads or columns. Although, some penicillate conidiophores are always<br />
present, Gliocladium species may also produce verticillate branching conidiophores<br />
which can be confused with Verticillium or Trichoderma.<br />
Gliocladium species have a world-wide distribution and are commonly isolated from a<br />
wide range of plant debris and soil. RG-1 organism.<br />
Key Features: hyphomycete producing distinctive erect penicillate conidiophores with<br />
phialides bearing clusters of single-celled conidia.<br />
For descriptions of species, keys to taxa and additional information see Domsch et al.<br />
(1980), McGinnis (1980), Onions et al. (1981), Rippon (1988), de Hoog et al. (2000).<br />
Conidiophore and conidia of Gliocladium.<br />
10 µm
74<br />
Descriptions of Medical Fungi<br />
Graphium Corda<br />
The genus Graphium is characterised by the formation of synnemata which consist of<br />
a more or less compact group of erect conidiophores that are cemented together, usually<br />
splaying out and bearing conidia at the apex. Synnemata are darkly pigmented,<br />
erect and occur solitary or in clusters. Conidia are hyaline, one-celled, smooth, subglobose<br />
to ovoid and are usually aggregated in slimy heads at the apex of the synnemata.<br />
Colonies are effuse, grey, olivaceous brown or black.<br />
Graphium eumorphum is one of the synanamorphs of Pseudallescheria boydii and is<br />
commonly found on woody plant material. RG-1 organism.<br />
Key Features: dematiaceous hyphomycete producing erect synnemata with apical<br />
aggregates of single-celled conidia in slimy heads.<br />
For descriptions of species, keys to taxa and additional information see Barron (1968),<br />
Ellis (1971), McGinnis (1980) and de Hoog et al. (2000).<br />
20 µm<br />
Synnemata and conidia of Graphium.
Descriptions of Medical Fungi 75<br />
Histoplasma capsulatum Darling<br />
Histoplasma capsulatum exhibits thermal dimorphism growing in living tissue or in culture<br />
at 37 O C as a budding yeast-like fungus and in soil or culture at temperatures below<br />
30 O C as a mould.<br />
Colonies (SDA) at 25 O C are slow growing, white or buff-brown, suede-like to cottony<br />
with a pale yellow-brown reverse. Other colony types are glabrous or verrucose, and a<br />
red pigmented strain has been noted (Rippon, 1988). Microscopic morphology shows<br />
the presence of characteristic large, rounded, single-celled, 8-14 µm in diameter, tuberculate<br />
macroconidia formed on short, hyaline, undifferentiated conidiophores. Small,<br />
round to pyriform, 2-4 µm in diameter, microconidia borne on short branches or directly<br />
on the sides of the hyphae may also be present.<br />
On brain heart infusion agar containing blood incubated at 37 O C colonies are smooth,<br />
moist, white and yeast-like. Microscopically, numerous small round to oval budding<br />
yeast-like cells, 3-4 x 2-3 µm in size are observed.<br />
Three varieties of Histoplasma capsulatum are recognised, depending on the clinical<br />
disease: var. capsulatum is the common cause of histoplasmosis; var. duboisii is the<br />
African type and var. farciminosum causes lymphangitis in horses. Histoplasma isolates<br />
may also resemble species of Sepedonium and Chrysosporium. Traditionally,<br />
positive identification required conversion of the mould form to the yeast phase by<br />
growth at 37 O C on enriched media, however culture identification by exoantigen test is<br />
now the method of choice.<br />
WARNING: RG-3 organism. Cultures of Histoplasma capsulatum represent a severe<br />
biohazard to laboratory personnel and must be handled with extreme caution in an<br />
appropriate pathogen handling cabinet.<br />
Key Features: clinical history, tissue morphology, culture morphology and positive<br />
exoantigen test.<br />
Histoplasma capsulatum has a world wide distribution, however the Mississippi-Ohio<br />
River Valley in the USA is recognised as a major endemic region. Environmental isolations<br />
of the fungus have been made from soil enriched with excreta from chicken, starlings<br />
and bats. Histoplasmosis is an intracellular mycotic infection of the reticuloendothelial<br />
system caused by the inhalation of the fungus. Approximately 95% of cases<br />
of histoplasmosis are inapparent, subclinical or benign. Five percent of the cases have<br />
chronic progressive lung disease, chronic cutaneous or systemic disease or an acute<br />
fulminating fatal systemic disease. All stages of this disease may mimic tuberculosis.<br />
Sporadic cases do occur in Australia.<br />
For descriptions of species, keys to taxa and additional information see McGinnis<br />
(1980), Chandler et al. (1980), George and Penn (1986), Rippon (1988) and de Hoog<br />
et al. (2000).
76<br />
Descriptions of Medical Fungi<br />
20 µm<br />
Culture and microscopic morphology of the saprophytic or mycelial form of<br />
H. capsulatum showing characteristic large, rounded, single-celled, tuberculate<br />
macroconidia formed on short, hyaline, undifferentiated conidiophores.<br />
Antifungal<br />
MIC µg/mL<br />
Range MIC90 Antifungal<br />
MIC µg/mL<br />
Range MIC90 Amphotericin B 0.03-2 0.5-1 Posaconazole 0.25-1 0.25 (2)<br />
Fluconazole 0.125-64 16 Voriconazole 0.03-2 0.25 (1)<br />
Itraconazole 0.03-8 0.06 (1)<br />
Histoplasma capsulatum Darling<br />
Limited data available. Espinel-Ingroff et al. (2001), Espinel-Ingroff (2003), Gonzales<br />
et al. (2005) and Sabatelli et al. (2006).
Descriptions of Medical Fungi 77<br />
Synonyms: Phaeoannellomyces werneckii (Horta) McGinnis & Schell<br />
Exophiala werneckii (Horta) v. Arx<br />
Colonies are slow growing, initially mucoid, yeast-like and shiny black. However with<br />
age they develop abundant aerial mycelia and become dark olivaceous in colour. Microscopically,<br />
colonies consist of brown to dark olivaceous, septate hyphal elements<br />
and numerous two-celled, pale brown, cylindrical to spindle-shaped yeast-like cells that<br />
taper towards the ends to form an annellide. Most yeast-like cells also have prominent<br />
darkly-pigmented septa. Annellides may also arise from the hyphae. Conidia are one<br />
to two-celled, cylindrical to spindle-shaped, hyaline to pale brown and usually occur in<br />
aggregated masses. RG-1 organism.<br />
Hortaea werneckii is a common saprophytic fungus believed to occur in soil, compost,<br />
humus and on wood in humid tropical and sub-tropical regions and is the causative<br />
agent of tinea nigra in humans.<br />
Key Features: dematiaceous hyphomycete, two-celled yeast-like cells producing<br />
annelloconidia.<br />
For description of species, keys to taxa and additional information see Mok (1982),<br />
McGinnis (1980), McGinnis et al. (1985), Rippon (1988) and de Hoog et al. (2000).<br />
Antifungal<br />
Hortaea werneckii (Horta) Nishimura & Miyaji<br />
Culture and conidia of Hortaea werneckii.<br />
20 µm<br />
MIC µg/mL MIC µg/mL MIC µg/mL<br />
Antifungal Antifungal<br />
Range Range Range<br />
Amphotericin B 0.03-1 Itraconazole 0.03-0.25 Voriconazole 0.03-0.125<br />
Very limited data, antifungal susceptibility testing of individual strains is recommended.<br />
McGinnis and Pasarell (1998) and WCH in-house data.
78<br />
Descriptions of Medical Fungi<br />
Lasiodiplodia theobromae (Pat.) Griffon & Maublanc<br />
Teleomorph: Botryosphaeria rhodina (Berk, & Curt. v. Arx<br />
Synonym: Botryodiplodia theobromae Patouillard<br />
Colonies are greyish sepia to mouse grey to black, fluffy with abundant aerial mycelium;<br />
reverse fuscous black to black. Pycnidia are simple or compound, often aggregated,<br />
stromatic, ostiolate, frequently setose, up to 5 mm wide. Conidiophores are hyaline,<br />
simple, sometimes septate, rarely branched cylindrical, arising from the inner layers of<br />
cells lining the pycnidial cavity. Conidiogenous cells are hyaline, simple, cylindrical to<br />
subobpyriform, holoblastic, annellidic. Conidia are initially unicellular, hyaline, granulose,<br />
subovoid to ellipsoide-oblong, thick-walled, base truncate; mature conidia oneseptate,<br />
cinnamon to fawn, often longitudinally striate, 20-30 x 10-15 µm. Paraphyses<br />
when present are hyaline, cylindrical, sometimes septate, up to 50 µm long.<br />
Lasiodiplodia theobromae is a well known plant pathogen and it has been reported<br />
from about 500 host plants, mainly confined to an area 40 O north to 40 O south of the<br />
equator. It has also been associated with mycotic keratitis, lesions on nail and subcutaneous<br />
tissue. RG-1 organism.<br />
Key Features: coelomycete, with pycnidia producing characteristic two-celled, dark<br />
brown, striated conidia.<br />
For description of species, keys to taxa and additional information see de Hoog et al.<br />
(2000).<br />
10 µm<br />
Mature two-celled dark brown conidia with typical striations of L. theobromae.<br />
Antifungal<br />
MIC µg/mL MIC µg/mL MIC µg/mL<br />
Antifungal Antifungal<br />
Range Range Range<br />
Amphotericin B 0.03 Itraconazole 16 Voriconazole 0.25<br />
Very limited data, antifungal susceptibility testing of individual strains is recommended.<br />
WCH in-house data only.
Descriptions of Medical Fungi 79<br />
Lecythophora Nannfeldt<br />
Colonies are pink to salmon, later becoming blackish, smooth, often mucoid or yeastlike.<br />
Conidiogenous cells are poorly differentiated, usually lateral or intercalary, hyphae<br />
bearing one or several scattered inconspicuous collarettes, either sessile or on small<br />
outgrowths. Conidia are hyaline, smooth and thin walled, broadly ellipsoidal, cylindrical,<br />
reniform or allantoid. Chlamydospores may be present. Lecythophora contains 6<br />
species, with two species of medical interest; L hoffmannii and L. mutabilis.<br />
Lecythophora hoffmannii (J.F.H. Beyma) W. Gams & McGinnis<br />
Teleomorph: Coniochaeta ligniaria (Grev.) Cooke<br />
Colonies are flat, smooth, moist, pink to orange, with regular and sharp margin; reverse<br />
pink. Hyphae are narrow, hyaline, producing conidia laterally from small collarettes<br />
directly on the hyphae, or from lateral cells which are sometimes arranged in dense<br />
groups; lateral cells flask-shaped or nearly cylindrical. Collarettes are unpigmented,<br />
about 1.5 µm wide. Conidia are hyaline, smooth and thin walled, broadly ellipsoidal to<br />
cylindrical or allantoid, 3.0-3.5 x 1.5-2.5 µm, produced in slimy heads. RG-1 organism.<br />
For description of species, keys to taxa and additional information see de Hoog (1983)<br />
and de Hoog et al. (2000).<br />
10 µm<br />
10 µm<br />
Culture, hyphae with small collarettes and conidia of Lecythophora hoffmannii.<br />
Antifungal<br />
MIC µg/mL MIC µg/mL MIC µg/mL<br />
Antifungal Antifungal<br />
Range Range Range<br />
Amphotericin B 0.06-0.5 Itraconazole 0.06-32 Voriconazole 0.125-0.5<br />
Very limited data, antifungal susceptibility testing of individual strains is recommended.<br />
McGinnis and Pasarell (1998).
80<br />
Descriptions of Medical Fungi<br />
Madurella grisea Mackinnon, Ferrada and Montemayer<br />
The genus Madurella is based on tissue morphology (mycetoma with black grains)<br />
and the formation of sterile cultures on mycological media. Both M. mycetomatis and<br />
M. grisea have been isolated from soil and are one of the major causative agents of<br />
mycetoma.<br />
Colonies are slow growing, dark, leathery, folded with radial grooves and with a light<br />
brown to greyish surface mycelium. With age, colonies become dark brown to reddish-brown<br />
and have a brownish-black reverse. Microscopically, cultures are sterile,<br />
although hyphae of two widths have been described, thin at 1-3 µm in width or broad at<br />
3-5 µm in width. The optimum temperature for growth of M. grisea is 30 O C; this fungus<br />
does not grow at 37 O C. RG-2 organism.<br />
M. grisea can be distinguished from Madurella mycetomatis by the inability to grow at<br />
37 O C and to assimilate lactose.<br />
Key Features: black grain mycetoma, no growth at 37 O C, no diffusible brown pigment<br />
produced on culture and absence of conidia.<br />
For descriptions of species, keys to taxa and additional information see McGinnis<br />
(1980), Chandler et al. (1980), Rippon (1988) and de Hoog et al. (2000).<br />
Antifungal<br />
100 µm<br />
Grains of Madurella grisea (tissue microcolonies) are black, round to<br />
lobed, soft to firm, up to 1.0 mm, with two distinctive zones, a hyaline to<br />
weakly pigmented central zone and a deeply pigmented periphery.<br />
MIC µg/mL MIC µg/mL MIC µg/mL<br />
Antifungal Antifungal<br />
Range Range Range<br />
Amphotericin B 0.25 Itraconazole 0.5 Voriconazole 0.5<br />
Very limited data, antifungal susceptibility testing of individual strains is recommended.<br />
Espinel-Ingroff et al. (2001).
Descriptions of Medical Fungi 81<br />
Madurella mycetomatis (Laveran) Brumpt<br />
Colonies are slow growing, flat and leathery at first, white to yellow to yellowish-brown,<br />
becoming brownish, folded and heaped with age and with the formation of aerial mycelia.<br />
A brown diffusible pigment is characteristically produced in primary cultures. Although<br />
most cultures are sterile, two types of conidiation have been observed, the first<br />
being flask-shaped phialides that bear rounded conidia, the second being simple or<br />
branched conidiophores bearing pyriform conidia (3-5 µm) with truncated bases. The<br />
optimum temperature for growth of this mould is 37 O C. RG-2 organism<br />
Grains of Madurella mycetomatis (tissue microcolonies) are brown or black, 0.5-1.0<br />
mm in size, round or lobed, hard and brittle, composed of hyphae which are 2-5 µm in<br />
diameter, with terminal cells expanded to 12-15 (30) µm in diameter.<br />
M. mycetomatis can be distinguished from Madurella grisea by growth at 37 O C and its<br />
inability to assimilate sucrose.<br />
Key Features: black grain mycetoma, growth at 37 O C, diffusible brown pigment<br />
produced on culture and the occasional presence of phialides.<br />
For descriptions of species, keys to taxa and additional information see McGinnis<br />
(1980), Chandler et al. (1980), Rippon (1988) and de Hoog et al. (2000).<br />
20 µm<br />
Culture showing brown diffusible pigment and phialides of M. mycetomatis.<br />
Antifungal<br />
MIC µg/mL MIC µg/mL MIC µg/mL<br />
Antifungal Antifungal<br />
Range Range Range<br />
Amphotericin B 0.03 Itraconazole 0.03-0.125 Voriconazole 0.03-0.6<br />
Very limited data, antifungal susceptibility testing of individual strains is recommended.<br />
McGinnis and Pasarell (1998) and Espinel-Ingroff et al. (2001).
82<br />
Descriptions of Medical Fungi<br />
Malassezia Baillon<br />
Malassezia is characterised by globose, oblong-ellipsoidal to cylindrical, yeast cells.<br />
Reproduction is by budding on a broad base and from the same site at one pole<br />
(unipolar). With the exception of M. pachydermatis, Malassezia are lipophilic yeasts,<br />
therefore in vitro growth must be stimulated by natural oils or other fatty substances.<br />
The most common method used is to overlay Sabouraud’s dextrose agar containing<br />
cycloheximide (actidione) with olive oil or alternatively to use a more specialised media<br />
like Dixon’s agar which contains glycerol mono-oleate. On such media, colonies are<br />
cream to yellowish, smooth or lightly wrinkled, glistening or dull, and with the margin<br />
being either entire or lobate (see photo). Seven species have now been recognised<br />
(Gueho et al. 1996). RG-2 organisms.<br />
Species Source<br />
M. furfur humans, normal flora, pityriasis<br />
M. globosa humans, normal flora, pityriasis<br />
M. pachydermatis animals, especially dogs<br />
M. obtusa humans, normal flora,<br />
atopic dermatitis<br />
M. restricta humans, normal flora<br />
M. slooffiae human and pig normal flora<br />
M. sympodialis humans, normal flora<br />
Identification criteria for the differentiation of Malassezia species (de Hoog et. al. 2000).<br />
Buds SDA 40 O C Cremophor<br />
EL<br />
Tween<br />
80<br />
Tween<br />
40<br />
Tween<br />
20<br />
Esculine Catalase<br />
M. furfur wide - + + + + + w +<br />
M. globosa narrow - - - - - - - +<br />
M. pachydermatis wide + + -,w + + -,w v v<br />
M. obtusa wide - - - - - - + +<br />
M. restricta narrow - - - - - - - -<br />
M. slooffiae wide - + - +,w + + - +<br />
M. sympodialis narrow - + -,w + + + + +<br />
For descriptions of species, keys to taxa and additional information see Guillot and<br />
Gueho (1995), Gueho et al. (1996), Guillot et al. (1996, 2000), de Hoog et al. (2000).<br />
Antifungal<br />
MIC µg/mL<br />
MIC µg/mL<br />
Range MIC90 Antifungal Range MIC90 Fluconazole 0.125->64 4 (8) Amphotericin B 0.03-16 1 (8)<br />
Itraconazole 0.03-16 0.125 Voriconazole 0.03-16 0.125 (1)<br />
Ketoconazole 0.03-4 0.25 Posaconazole 0.03-32 0.125 (2)<br />
Very limited data available. Special growth conditions are needed for antifungal<br />
susceptibility testing. Nakamura et al. (2000), Velegraki et al. (2004) and Miranda et<br />
al. (2007).
Descriptions of Medical Fungi 83<br />
Malbranchea Saccardo<br />
Colonies are white to sulphur-yellow to ochre-brown in colour, suede-like in texture,<br />
with a reddish-brown reverse, and often a reddish diffusible pigment. Microscopic morphology<br />
shows typical hyaline, one-celled, cylindrical, truncate, alternate arthroconidia<br />
produced in terminal fertile portions of the hyphae. Arthroconidia are released by lysis<br />
of the disjunctor cells. These arthroconidia may be perceived as a yellow dust when<br />
released at maturity. RG-1 organisms.<br />
Key Features: hyphomycete producing alternate arthroconidia with disjunctor cells.<br />
Malbranchea species are soil fungi of world-wide distribution which microscopically<br />
may resemble Coccidioides immitis/posadasii. Exoantigen tests are now the method<br />
of choice for culture identification of C. immitis/posadasii.<br />
For description of the species, keys to taxa and additional information see Cooney and<br />
Emerson (1964), McGinnis (1980), Rippon (1988) and de Hoog et al. (2000).<br />
20 µm<br />
Arthroconidia of Malbranchea.
84<br />
Descriptions of Medical Fungi<br />
Microsporum Gruby<br />
Teleomorph: Arthroderma Currey and Berkeley emend Weitzman et al.<br />
Microsporum species form both macro- and microconidia on short conidiophores.<br />
Macroconidia are hyaline, multiseptate, variable in form, fusiform, spindle-shaped to<br />
obovate, ranging from 7-20 x 30-60 µm in size, with thin- or thick- echinulate to verrucose<br />
cell walls. Their shape, size and cell wall features are important characteristics<br />
for species identification. Microconidia are hyaline, single-celled, pyriform to clavate,<br />
smooth-walled, 2.5-3.5 x 4-7 µm in size and are not diagnostic for any one species.<br />
The separation of this genus from Trichophyton is essentially based on the roughness<br />
of the macroconidial cell wall, although in practice this may sometimes be difficult to<br />
observe. Seventeen species of Microsporum have been described (Rippon, 1988)<br />
however only the more common species are included in these descriptions.<br />
It is essential to observe macroconidia when identifying species of Microsporum.<br />
Strains of M. canis often do not produce macroconidia and/or microconidia on primary<br />
isolation media and it is recommended that sub-cultures be made onto polished rice<br />
grains to stimulate sporulation. These non-sporulating strains of M. canis are often<br />
erroneously identified as M. audouinii and it is surprising just how many laboratories<br />
have difficulty in differentiating between M. canis and M. audouinii.<br />
For descriptions of species, keys to taxa and additional information see Rebell and<br />
Taplin (1970), Vanbreusegham et al. (1978), Rippon (1988), McGinnis (1980), Domsch<br />
et al. (1980), Ajello (1977), Weitzman et al. (1986), Mackenzie et al. (1986), Kane et al.<br />
(1997) and de Hoog et al. (2000).<br />
a<br />
(a) M. audouinii showing poor growth on rice grains, usually being visible only<br />
as a brown discolouration. (b) M. canis on rice grains showing good growth,<br />
yellow pigmentation and sporulation.<br />
Antifungal<br />
MIC µg/mL<br />
MIC µg/mL<br />
Range MIC90 Antifungal Range MIC90 Griseofulvin 0.125-2 1 Amphotericin B 0.03-8 1-2<br />
Itraconazole 0.01-4 0.25-0.5 Fluconazole 0.06->64 64<br />
Terbinafine 0.01-16 0.06 Voriconazole 0.007-1 0.5<br />
Fernandez-Torres et al. (2001), Sabatelli et al. (2006) and WCH in-house data.<br />
b
Descriptions of Medical Fungi 85<br />
Microsporum audouinii Gruby<br />
Colonies (SDA) are flat, spreading, greyish-white to light tan-white in colour, and have<br />
a dense suede-like to downy surface, suggestive of mouse fur in texture. Reverse<br />
can be yellow-brown to reddish-brown in colour. Some strains may show no reverse<br />
pigment. Macroconidia and microconidia are only rarely produced, most cultures are<br />
sterile or produce only occasional thick-walled terminal or intercalary chlamydospores.<br />
When present macroconidia may resemble those of M. canis but are usually longer,<br />
smoother and more irregularly fusiform in shape; microconidia when present are pyriform<br />
to clavate in shape and are similar to those seen in other species of Microsporum.<br />
So called pectinate (comb-like) hyphae and racquet hyphae (a series of hyphal segments<br />
swollen at one end) may also be present. RG-2 organism.<br />
Culture and a thick-walled intercalary chlamydospore of M. audouinii. Note:<br />
macroconidia and microconidia are only rarely produced.<br />
Growth on Rice Grains: Very poor or absent, usually being visible only as a brown<br />
discolouration. This is one of the features which distinguish M. audouinii from M.<br />
canis.<br />
Reverse Pigment on Potato Dextrose Agar: Salmon to pinkish-brown (M. canis is<br />
bright yellow).<br />
Lactritmel Agar: Colonies are usually flat, spreading, with a fine, whitish suede-like<br />
surface and a very pale yellow-brown reverse. Microscopic morphology as described<br />
above.<br />
Vitamin Free Agar (Trichophyton Agar No.1): Good growth indicating no special<br />
nutritional requirements. Cultures are flat, white, suede-like to downy, with a yellowbrown<br />
reverse. Note: growth of some strains of M. audouinii is enhanced by the presence<br />
of thiamine (Trichophyton agar No.4).<br />
Hair Perforation Test: Negative after 28 days.<br />
10 µm<br />
Key Features: absence of conidia, poor or no growth on polished rice grains, inability<br />
to perforate hair in vitro, and culture characteristics.<br />
M. audouinii is an anthropophilic fungus causing non-inflammatory infections of scalp<br />
and skin especially in children. Once the cause of epidemics of tinea capitis in Europe<br />
and North America, it is now becoming less frequent. Invaded hairs show an ectothrix<br />
infection and usually fluoresce a bright greenish-yellow under Wood’s ultra-violet light.<br />
Only rarely found in Australasia, most reports are in fact non-sporulating strains of M.<br />
canis.
86<br />
Descriptions of Medical Fungi<br />
Microsporum canis Bodin<br />
Teleomorph: Arthroderma otae (Hasegawa and Usui) McGinnis, et al.<br />
Colonies (SDA) are flat, spreading, white to cream-coloured, with a dense cottony<br />
surface which may show some radial grooves. Colonies usually have a bright golden<br />
yellow to brownish yellow reverse pigment, but non-pigmented strains may also occur.<br />
Macroconidia are typically spindle-shaped with 5-15 cells, verrucose, thick-walled and<br />
often have a terminal knob, 35-110 x 12-25 µm. A few pyriform to clavate microconidia<br />
are also present. Macroconidia and/or microconidia are often not produced on primary<br />
isolation media and it is recommended that sub-cultures be made onto Lactritmel Agar<br />
and/or boiled polished rice grains to stimulate sporulation. RG-2 organism.<br />
Growth on Rice Grains: good growth of white aerial mycelium with production of yellow<br />
pigment. Microscopy reveals numerous macroconidia and microconidia similar to<br />
those described above.<br />
Lactritmel Agar: Flat, white suede-like to cottony colony with a bright yellow reverse.<br />
Microscopy reveals moderate numbers of thick-walled, multiseptate, long, spindleshaped<br />
macroconidia, some of which show a terminal knob. Walls of macroconidia<br />
are slightly rough or echinulate especially at terminal knobs. Numerous clavate to<br />
pyriform microconidia are also present in this strain. Lactritmel agar with sterile soil<br />
added is also an excellent medium for the stimulation of macroconidial development<br />
in M. canis.<br />
Reverse Pigment on Potato Dextrose Agar: Bright yellow (both M. audouinii and M.<br />
canis var. equinum are salmon to pinkish-brown).<br />
Vitamin Free Agar (Trichophyton Agar No.1): Good growth indicating no special<br />
nutritional requirements. Cultures are flat, white, suede-like to downy, with a yellow to<br />
pale yellow-brown reverse.<br />
Hair Perforation Test: Positive at 14 days.<br />
Key Features: distinctive macroconidia and culture characteristics. Abundant growth<br />
and sporulation on polished rice grains and in vitro perforation of hair.<br />
Culture of Microsporum canis.
Descriptions of Medical Fungi 87<br />
Microsporum canis Bodin<br />
Typical spindle-shaped macroconidia of Microsporum canis.<br />
20 µm<br />
Dysgonic strains of M. canis are rare but may also occur. These dysgonic strains have<br />
a typically heaped and folded, yellow-brown thallus and macroconidia are usually<br />
absent. However, typical colonies and macroconidia of M. canis are usually produced<br />
by this variant when subcultured onto polished rice grains. Note: the dysgonic type<br />
colony of M. canis is similar to that of Microsporum ferrugineum.<br />
M. canis is a zoophilic dermatophyte of world-wide distribution and is a frequent cause<br />
of ringworm in humans, especially children. Invades hair, skin and rarely nails. Cats<br />
and dogs are the main sources of infection. Invaded hairs show an ectothrix infection<br />
and fluoresce a bright greenish-yellow under Wood’s ultra-violet light.
88<br />
Descriptions of Medical Fungi<br />
Microsporum canis var. distortum di Menna & Marples<br />
Supplementary description for Microsporum canis var. distortum, a dysgonic variant of<br />
M. canis with distinctive distorted macroconidia. Abundant growth and sporulation on<br />
rice grains. RG-2 organism.<br />
Microsporum canis var. distortum is a zoophilic fungus known to cause infections in<br />
cats, dogs and other animals. It is a rare cause of tinea capitis in New Zealand,<br />
Australia and North America. Clinical disease is similar to M. canis . Invaded hairs<br />
show an ectothrix infection and fluoresce a bright greenish-yellow under Wood’s ultraviolet<br />
light.<br />
20 µm<br />
Culture and distorted macroconidia of M. canis var. distortum.
Descriptions of Medical Fungi 89<br />
Microsporum canis var. equinum (Delacroix & Bodin) comb. nov.<br />
Basionym: Microsporum equinum (Delacroix & Bodin) Gueguen<br />
Microsporum equinum is now considered to be a genotypic synonym of Microsporum<br />
canis (de Hoog et al. 2000), however we propose it be maintained as a variety of M.<br />
canis due to phenotypic and epidemiologic differences.<br />
Colonies are flat, spreading, suede-like, pale buff to pale salmon, usually with some radial<br />
furrows. A buff to pinkish-buff to yellow-brown reverse pigment is produced. Note:<br />
only a few strains produce conidia on primary isolation, however growth on urea agar<br />
usually stimulates the production of macroconidia. Macroconidia are small (especially<br />
when compared to those produced by M. canis), broad, irregular, spindle-shaped, 18-<br />
60 x 5-15 mm with rough thick walls and few septa. Microconidia are pyriform to clavate<br />
in shape, 3-9 x 1.5-3.5 mm, but are rarely produced. RG-2 organism.<br />
Growth on Rice Grains: Poor with minimal surface growth, usually being visible only<br />
as a brown discolouration. This is one of the features which distinguish M. canis var.<br />
equinum from M. canis.<br />
Reverse Pigment on Potato Dextrose Agar: Salmon to pinkish-brown (M. canis is<br />
bright yellow).<br />
Lactritmel Agar: Colonies are usually flat, spreading, with a fine, whitish suede-like<br />
surface and a very pale yellow-brown reverse. Microscopic morphology as described<br />
above.<br />
Vitamin Free Agar (Trichophyton Agar No.1): Good growth indicating no special<br />
nutritional requirements. Cultures are flat, white, suede-like to downy, with a yellowbrown<br />
reverse.<br />
Hair Perforation Test: Negative after 28 days.<br />
Key Features: macroconidial shape and size, inability to perforate hair in vitro, and<br />
poor growth on polished rice grains.<br />
20 µm<br />
Culture and macroconidia of M. canis var. equinum.<br />
Microsporum equinum is a<br />
rare cause of ringworm of<br />
horses. Invaded hairs show<br />
an ectothrix infection and<br />
fluoresce a bright greenishyellow<br />
under Wood’s ultraviolet<br />
light. Rarely infects<br />
man or other animal species.<br />
Reported from Australia,<br />
Europe and North America.
90<br />
Descriptions of Medical Fungi<br />
Teleomorph: Arthroderma cajetani Ajello, Weitzman, McGinnis & Padhye<br />
Colonies (SDA) are flat, spreading, buff to pale brown, powdery to suede-like, with a<br />
slightly raised and folded centre and some radial grooves. Reverse pigment dark reddish<br />
brown. Numerous large, very thick-walled, echinulate (rough) elliptical macroconidia<br />
with predominantly 5-6 septa but may be 2-8 septate. Occasional spirals may be<br />
seen. Moderate numbers of mainly slender clavate with some pyriform microconidia<br />
are present. The macroconidia are quite characteristic and diagnostic of M. cookei and<br />
further tests are not necessary. The thick walls and usually larger size of the macroconidia<br />
distinguish M. cookei from M. gypseum. RG-1 organism.<br />
Lactritmel Agar: Flat, buff-coloured, suede-like to powdery colony with a deep redbrown<br />
reverse. Microscopic morphology as described above for the primary culture.<br />
Vitamin Free Agar (Trichophyton Agar No.1): Good growth indicating no special<br />
nutritional requirements, pinkish-buff-coloured, suede-like colony with a deep magenta<br />
red reverse.<br />
Hair Perforation Test: Positive.<br />
Microsporum cookei Ajello<br />
Key Features: distinctive macroconidial morphology and culture characteristics.<br />
20 µm<br />
Culture and macroconidia of Microsporum cookei.<br />
Microsporum cookei is a geophilic fungus which has been isolated from hair of small<br />
mammals showing no clinical lesions. Infection has been reported in rodents, dogs<br />
and rarely in humans. It is not known to invade hair in vivo, but produces hair perforations<br />
in vitro. M. cookei has a world-wide distribution.
Descriptions of Medical Fungi 91<br />
Microsporum ferrugineum Ota<br />
Colonies (SDA) are slow growing, forming a waxy, glabrous, convoluted thallus with a<br />
cream to buff-coloured surface and no reverse pigment. Note: surface pigmentation<br />
may vary from cream to yellow to deep red and a flatter white form sometimes occurs.<br />
Cultures rapidly become downy and pleomorphic. Microconidia or macroconidia are<br />
not produced. However, irregular branching hyphae with prominent cross walls (“bamboo<br />
hyphae”) and chlamydospores are seen. The so-called “bamboo hyphae” is a<br />
characteristic of this species. RG-2 organism.<br />
Key Features: clinical history, culture characteristics and distinctive “bamboo”<br />
hyphae.<br />
20 µm<br />
Culture and “bamboo hyphae” of Microsporum ferrugineum.<br />
Microsporum ferrugineum is an anthropophilic fungus causing epidemic juvenile tinea<br />
capitis in humans. The clinical features are similar to those of infections caused by<br />
M. audouinii. Invaded hairs show an ectothrix infection and fluoresce a greenish-yellow<br />
under Wood’s ultra-violet light. Reported from Asia (including China and Japan),<br />
USSR, Eastern Europe and Africa.
92<br />
Descriptions of Medical Fungi<br />
Microsporum fulvum Uriburu<br />
Teleomorph: Arthroderma fulvum (Stockdale) Weitzman et al.<br />
Colonies (SDA) are fast growing, flat, suede-like, tawny-buff to pinkish-buff in colour and<br />
frequently have a fluffy white advancing edge. A dark red under surface is occasionally<br />
seen, otherwise it is colourless to yellow brown. Abundant thin-walled, elongate, ellipsoidal<br />
macroconidia are formed which closely resemble those of M. gypseum, except<br />
they are longer and more bullet-shaped (clavate) with 3 to 6 septa. Numerous spiral<br />
hyphae, which are often branched are seen. Numerous pyriform to clavate microconidia<br />
are also produced but these are not diagnostic. RG-1 organism.<br />
Key Features: macroconidial morphology and culture characteristics.<br />
20 µm<br />
Culture and macroconidia of Microsporum fulvum.<br />
Microsporum fulvum is a geophilic fungus of world-wide distribution which may cause<br />
occasional infections in humans and animals. Clinical disease is similar to M. gypseum<br />
but less common. Invaded hairs show a sparse ectothrix infection but do not fluoresce<br />
under Wood’s ultra-violet light.
Descriptions of Medical Fungi 93<br />
Microsporum gallinae (Megnin) Grigorakis<br />
Colonies (SDA) are flat with a suede-like texture and are white in colour with a pinkish<br />
tinge. Some cultures show radial folding. An orange-pink “strawberry-coloured”<br />
reverse pigment is usually present. Macroconidia when present are usually five- to sixcelled,<br />
thin to thick-walled, slightly echinulate, cylindrical to clavate with narrow base<br />
and blunt tip, 15-60 x 6-10 µm. Microconidia are ovoidal to pyriform in shape. RG-2<br />
organism.<br />
Key Features: macroconidial morphology, culture characteristics and clinical lesions<br />
in chickens.<br />
Culture and macroconidia of Microsporum gallinae.<br />
20 µm<br />
Microsporum gallinae is a zoophilic fungus causing fowl favus in chickens and other<br />
fowl, affecting the comb and wattles producing “white comb” lesions. A rare cause of<br />
tinea in humans. Invaded hairs show a sparse ectothrix infection but do not fluoresce<br />
under Wood’s ultra-violet light.
94<br />
Descriptions of Medical Fungi<br />
Microsporum gypseum (Bodin) Guiart & Grigorakis<br />
Teleomorphs: Arthroderma gypsea (Nannizzi) Weitzman et al.<br />
Arthroderma incurvatum (Stockdale) Weitzman et al.<br />
Colonies (SDA) are usually flat, spreading, suede-like to granular, with a deep cream<br />
to tawny-buff to pale cinnamon-coloured surface. Many cultures develop a central<br />
white downy umbo (dome) or a fluffy white tuft of mycelium and some also have a narrow<br />
white peripheral border. A yellow-brown pigment, often with a central darker brown<br />
spot, is usually produced on the reverse, however a reddish-brown reverse pigment<br />
may be present in some strains. Cultures produce abundant, symmetrical, ellipsoidal,<br />
thin-walled, verrucose, four- to six-celled macroconidia. The terminal or distal ends of<br />
most macroconidia are slightly rounded, while the proximal ends (point of attachment<br />
to hyphae) are truncate. Numerous clavate-shaped microconidia are also present, but<br />
these are not diagnostic. RG-1 organism.<br />
Key Features: distinctive macroconidia and culture characteristics.<br />
20 µm<br />
Culture and macroconidia of Microsporum gypseum.<br />
Microsporum gypseum is a geophilic fungus with a world-wide distribution which may<br />
cause infections in animals and humans, particularly children and rural workers during<br />
warm humid weather. Usually produces a single inflammatory skin or scalp lesion. Invaded<br />
hairs show an ectothrix infection but do not fluoresce under Wood’s ultra-violet<br />
light.
Descriptions of Medical Fungi 95<br />
Microsporum nanum Fuentes<br />
Teleomorph: Arthroderma obtusum (Dawson and Gentles) Weitzman et al.<br />
Colonies (SDA) are flat, cream to buff in colour with a suede-like to powdery surface<br />
texture. Young colonies have a brownish-orange pigment which deepens into a dark<br />
reddish-brown with age. Cultures produce numerous small ovoid to pyriform macroconidia<br />
with one to three (mostly 2) cells, with relatively thin, finely echinulate (rough)<br />
walls, and broad truncate bases. Many macroconidia are borne on conidiophores<br />
(stalks) which do not stain readily. Occasional clavate microconidia are present, which<br />
distinguishes M. nanum from some species of Chrysosporium. RG-2 organism.<br />
Key Features: distinctive macroconidia and culture characteristics.<br />
20 µm<br />
Culture and macroconidia of Microsporum nanum.<br />
Microsporum nanum is a geophilic and zoophilic fungus frequently causing chronic<br />
non-inflammatory lesions in pigs and a rare cause of tinea in humans. Also present in<br />
soil of pig-yards. Infections in man are usually contacted directly from pig or fomites.<br />
Invaded hairs may show a sparse ectothrix or endothrix infection but do not fluoresce<br />
under Wood’s ultra-violet light. The geographical distribution is world-wide.
96<br />
Descriptions of Medical Fungi<br />
Microsporum persicolor (Sabouraud) Guiart & Grigorakis<br />
Teleomorph: Arthroderma persicolor (Stockdale) Weitzman et al.<br />
Colonies (SDA) are generally flat, white to pinkish in colour, with a suede-like to granular<br />
texture and peripheral fringe. Reverse pigmentation is orange to red. Macroconidia<br />
are thin-walled, cigar-shaped, four- to seven-celled, 40-60 x 6-8 µm but are only rarely<br />
produced. Microconidia are abundant, spherical to pyriform. RG-2 organism.<br />
Key Features: microscopic morphology and culture characteristics.<br />
Culture and microconidia of Microsporum persicolor.<br />
20 µm<br />
Microsporum persicolor is a zoophilic fungus often occurring as a saprophyte on voles<br />
and bats. A rare cause of tinea corporis in humans. Not known to invade hair in<br />
vivo, but produces hair perforations in vitro. Distribution: Africa, Australia, Europe and<br />
North America.
Descriptions of Medical Fungi 97<br />
Mortierella wolfii Mehrotra & Baijal<br />
The genus Mortierella has now been placed in a separate order, the Mortierellales<br />
(Cavalier-Smith 1998), and the genus contains about 90 recognised species, however<br />
Mortierella wolfii is probably the only pathogenic species being an important causal<br />
agent of bovine mycotic abortion, pneumonia and systemic mycosis in New Zealand,<br />
Australia, Europe and USA.<br />
Cultures are fast growing, white to greyish white, downy, often with a broadly zonate<br />
or lobed (rosette-like) surface appearance and no reverse pigment. Sporangiophores<br />
are typically erect, delicate, 80-250 µm in height, 6-20 µm wide at the base, arising<br />
from rhizoids or bulbous swellings on the substrate hyphae and terminating with<br />
a compact cluster of short acrotonous (terminal) branches. Sporangia are usually<br />
15-48 µm in diameter, with transparent walls and a conspicuous collarette is usually<br />
present following dehiscence of the sporangiospores. Columella are generally lacking<br />
and sporangiospores are single-celled, short-cylindrical, 6-10 x 3-5 µm, with a double<br />
membrane. Chlamydospores with or without blunt appendages (amoeba-like) may be<br />
present, zygospores have not been observed. Temperature: grows well at 40-42 O C;<br />
maximum 48 O C. RG-2 organism.<br />
Key Features: zygomycete, rapid growth at 40 O C (thermotolerant), and characteristic<br />
delicate acrotonous branching sporangia without columellae.<br />
For descriptions of species, keys to taxa and additional information see Domsch et al.<br />
(1980), McGinnis (1980), Rippon (1988), Smith (1989) and de Hoog et al. (2000).<br />
20 µm<br />
20 µm<br />
Culture of M. wolfii showing a broadly zonate or lobed rosette-like surface appearance<br />
and sporangium, showing a sporangiophore, wide at the base, arising from rhizoids,<br />
and acrotonous (terminal) branches, collarettes and sporangiospores.
98<br />
Descriptions of Medical Fungi<br />
Mucor Micheli ex Staint-Amans<br />
The genus Mucor can be differentiated from Absidia, Rhizomucor and Rhizopus by the<br />
absence of stolons and rhizoids. Colonies are very fast growing, cottony to fluffy, white<br />
to yellow, becoming dark-grey, with the development of sporangia. Sporangiophores<br />
are erect, simple or branched, forming large (60-300 µm in diameter), terminal, globose<br />
to spherical, multispored sporangia, without apophyses and with well-developed<br />
subtending columellae. A conspicuous collarette (remnants of the sporangial wall) is<br />
usually visible at the base of the columella after sporangiospore dispersal. Sporangiospores<br />
are hyaline, grey or brownish, globose to ellipsoidal, and smooth-walled or<br />
finely ornamented. Chlamydospores and zygospores may also be present.<br />
Key Features: zygomycete, large, spherical, non-apophysate sporangia with pronounced<br />
columellae and conspicuous collarette at the base of the columella following<br />
sporangiospore dispersal.<br />
Antifungal<br />
20 µm 20 µm<br />
Sporangia, columella with a conspicuous collarette (arrow)<br />
and sporangiospores of Mucor.<br />
MIC µg/mL<br />
MIC µg/mL<br />
Range MIC<br />
Antifungal<br />
Range MIC 90 90<br />
Fluconazole >64 >64 Amphotericin B 0.03-4 1<br />
Itraconazole 0.125-8 2 Flucytosine >256 >256<br />
Posaconazole 0.06-8 1 Voriconazole 8->64 >64<br />
Very limited data, antifungal susceptibility testing of individual strains is recommended.<br />
Sun et al. (2002), Dannaoui et al. (2003), Espinel-Ingroff (2001, 2003), Singh et al.<br />
(2005), Sabatelli et al. (2006) and WCH in-house data.
Descriptions of Medical Fungi 99<br />
Mucor Micheli ex Staint-Amans<br />
The genus Mucor contains about 50 recognised taxa, many of which have widespread<br />
occurrence and are of considerable economic importance (Zycha et al. 1969, Schipper<br />
1978, Domsch et al. 1980). However, only a few thermotolerant species are of<br />
medical importance and human infections are only rarely reported. Most infections<br />
reported list M. circinelloides and similar species such as M. indicus (M. rouxii), M. ramosissimus<br />
and M. amphibiorum as the causative agents. However, M. hiemalis and<br />
M. racemosus have also been reported as infectious agents, although their inability to<br />
grow at temperatures above 32 O C raises doubt as to their validity as human pathogens<br />
and their pathogenic role may be limited to cutaneous infections (Scholer et al. 1983,<br />
Goodman and Rinaldi 1991, Kwon-Chung and Bennett 1992, de Hoog et al. 2000).<br />
Maximum temperature for growth of the reported pathogenic species of Mucor.<br />
Species Max temp. ( O C) Pathogenicity<br />
M. amphibiorum 36 Animals, principally amphibians<br />
M. circinelloides 36-40 Animals, occasionally humans<br />
M. hiemalis 30 Questionable cutaneous infections only<br />
M. indicus 42 Humans and animals<br />
M. racemosus 32 Questionable<br />
M. ramosissimus 36 Humans and animals<br />
For descriptions of species, keys to taxa and additional information see Schipper<br />
(1978), Domsch et al. (1980), McGinnis (1980), Onions et al. (1981), Scholer et al.<br />
(1983), Rippon (1988), Goodman and Rinaldi (1991), Samson et al. (1995), de Hoog<br />
et al. (2000), Schipper and Staplers (2003) and Ellis (2005b).<br />
Mucor amphibiorum Schipper<br />
Colonies are greyish-brown, slightly aromatic and do not grow at 37 O C (maximum<br />
temperature for growth is 36 O C). Sporangiophores are hyaline, erect and mostly unbranched,<br />
rarely sympodially branched. Sporangia are dark-brown, up to 75 µm in<br />
diameter, and are slightly flattened with a diffluent membrane. Columellae are subglobose<br />
to ellipsoidal or pyriform, up to 60 x 50 µm, with small collarettes. Sporangiospores<br />
are smooth-walled, spherical, and 3.5-5.5 µm in diameter. Zygospores,<br />
when formed by compatible mating types, are spherical to slightly compressed, up to<br />
70 x 60 µm in diameter, with stellate projections. Mucor amphibiorum is distinguished<br />
by poor ramification of the sporangiophores and by globose sporangiospores. Ethanol<br />
and nitrate are not assimilated (Schipper 1978, Scholer et al. 1983, Hoog et al. 2000).<br />
RG-2 organism.
100<br />
Descriptions of Medical Fungi<br />
Mucor circinelloides v. Tiegh<br />
M. circinelloides is a common and variable species that includes 4 forms: circinelloides,<br />
lusitanicus, griseo-cyanus and janssenii (Schipper 1978, Scholer et al. 1983). Colonies<br />
are floccose, pale greyish-brown and grow poorly at 37 O C (maximum growth temperature<br />
36-40 O C). Sporangiophores are hyaline and mostly sympodially branched with<br />
long branches erect and shorter branches becoming circinate (recurved). Sporangia<br />
are spherical, varying from 20-80 µm in diameter, with small sporangia often having a<br />
persistent sporangial wall. Columellae are spherical to ellipsoidal and are up to 50 µm<br />
in diameter. Sporangiospores are hyaline, smooth-walled, ellipsoidal, and 4.5-7 x 3.5-<br />
5 µm in size. Chlamydospores are generally absent. Zygospores are only produced<br />
in crosses of compatible mating types and are reddish-brown to dark-brown, spherical<br />
with stellate spines, up to 100 µm in diameter and have equal to slightly unequal suspensor<br />
cells. M. circinelloides differs from other species of Mucor in its formation of<br />
short circinated (coiled), branched sporangiophores bearing brown sporangia and its<br />
ability to assimilate ethanol and nitrate (Schipper 1976, Scholer et al. 1983, Samson et<br />
al. 1995, de Hoog et al. 2000, Schipper and Staplers 2003). RG-1 organism.<br />
Mucor indicus Lendner<br />
Colonies are characteristically deep-yellow, aromatic and have a maximum growth<br />
temperature of 42 O C. Sporangiophores are hyaline to yellowish, erect or rarely circinate<br />
and repeatedly sympodially branched, with long branches. Sporangia are yellow<br />
to brown, up to 75 µm in diameter, with diffluent membranes. Columellae are subglobose<br />
to pyriform, often with truncate bases, up to 40 µm high. Sporangiospores are<br />
smooth-walled, subglobose to ellipsoidal, and 4-5 µm in diameter. Chlamydospores<br />
are produced in abundance, especially in the light. Zygospores when formed by crosses<br />
of compatible mating strains are black, spherical up to 100 µm in diameter, with<br />
stellate spines and unequal suspensor cells. Mucor indicus differs from other species<br />
of Mucor by its characteristic deep-yellow colony colour, growth at over 40 O C, assimilating<br />
ethanol, but not nitrate, and being thiamine dependent (Schipper 1978, de Hoog<br />
et al. 2000, Schipper and Staplers 2003). RG-1 organism.<br />
Mucor ramosissimus Samutsevich<br />
Colonial growth is restricted, greyish and does not grow at 37 O C (maximum temperature<br />
for growth is 36 O C). Sporangiophores are hyaline, slightly roughened, tapering<br />
towards the apex and are erect with repeated sympodial branching. Sporangia are<br />
grey to black, globose or somewhat flattened, up to 80 µm in diameter and have very<br />
persistent sporangial walls. Columellae are applanate (flattened), up to 40-50 µm in<br />
size and are often absent in smaller sporangia. Sporangiospores are faintly brown,<br />
smooth-walled, subglobose to broadly ellipsoidal, 5-8 x 4.5-6 µm in size. Oidia may be<br />
present in the substrate hyphae, chlamydospores and zygospores are absent. Assimilation<br />
of ethanol is negative and that of nitrate is positive. Mucor ramosissimus differs<br />
from other species of Mucor by its low, restricted growth on any medium, extremely persistent<br />
sporangial walls, columellae that are applanate or absent in smaller sporangia<br />
(often resembling Mortierella species), short sporangiophores that repeatedly branch<br />
sympodially as many as 12 times, and the occurrence of racket-shaped enlargements<br />
in the sporangiophores (Hesseltine and Ellis 1964, Schipper 1976, Scholer et al. 1983,<br />
de Hoog et al. 2000, Schipper and Staplers 2003). RG-1 organism.
Descriptions of Medical Fungi 101<br />
Nattrassia mangiferae (H. Syd. & Syd) Sutton & Dyko<br />
Pycnidial synanamorph: Hendersonula toruloidea Nattras<br />
Arthroconidial synanamorph: Scytalidium dimidiatum (Penzig) Sutton & Dyko<br />
Scytalidium hyalinum Campbell & Mulder<br />
This coelomycete is characterised by the presence of black, ostiolate pycnidia containing<br />
numerous hyaline, flask-shaped phialides. Phialoconidia are at first one-celled and<br />
hyaline, later becoming three-celled and brown, with the centre cell darker than the end<br />
cells. Conidia are ovoid to ellipsoidal in shape. Pycnidia are only occasionally formed<br />
in older cultures. In culture the Scytalidium dimidiatum anamorph is typically present<br />
showing chains of one- to two-celled, darkly pigmented arthroconidia, 3.5-5 x 6.5-12<br />
µm, produced by the holothallic fragmentation of undifferentiated hyphae. Cultures are<br />
effuse, hairy, dark grey to blackish-brown, or white to greyish, with a cream-coloured to<br />
deep ochraceous-yellow colony reverse. Colourless (hyaline) mutants (=Scytalidium<br />
hyalinum) often occur.<br />
Nattrassia mangiferae (arthric synanamorph = Scytalidium dimidiatum) is a recognised<br />
agent of onychomycosis and superficial skin infections, especially in tropical regions.<br />
However, isolates are sensitive to cycloheximide (actidione) which is commonly added<br />
to primary isolation media used for culturing skin scrapings. RG-2 organism.<br />
For descriptions of species, keys to taxa and additional information see McGinnis<br />
(1980), Moore (1986), Rippon (1988), Frankel and Rippon (1989), Sutton and Dyko<br />
(1989) and de Hoog et al. (2000).<br />
20 µm<br />
Microscopic morphology of the Scytalidium dimidiatum synanamorph of Nattrassia<br />
mangiferae showing chains of one- to two-celled, darkly pigmented<br />
arthroconidia.<br />
Antifungal<br />
MIC µg/mL MIC µg/mL MIC µg/mL<br />
Antifungal Antifungal<br />
Range Range Range<br />
Amphotericin B 0.125-2 Itraconazole 0.03-32 Voriconazole 0.03-0.5<br />
Very limited data, antifungal susceptibility testing of individual strains is recommended.<br />
Espinel-Ingroff et al. (2001) and WCH in-house data.
102<br />
Descriptions of Medical Fungi<br />
Ochroconis gallopava (W.B. Cooke) de Hoog<br />
Colonies are smooth to suede-like, dry, flat, tobacco-brown to brownish-black with a<br />
dark brown diffusible pigment. Hyphae are brown with relatively thick walls. Conidiophores<br />
are mostly cylindrical to acicular, sometimes poorly differentiated, bearing a few<br />
conidia at the tip. Conidia are two-celled, subhyaline to pale brown, smooth-walled to<br />
verrucose, cylindrical to clavate, constricted at the septum, 11-18 x 2.5-4.5 µm in size,<br />
with the apical cell wider than the basal cell. A remnant of a denticle may also be seen<br />
at the conidial base. Optimum growth at 35 O C, tolerant to 40 O C. RG-2 organism.<br />
Ochroconis gallopava is a well recognised species and has been reported as an<br />
avian pathogen, especially in poultry. Occasional human infections have also been<br />
reported.<br />
For descriptions of species, keys to taxa and additional information see Domsch et al.<br />
1980, McGinnis 1980 and de Hoog et al. 2000.<br />
Antifungal<br />
10 µm<br />
10 µm<br />
Hyphae, conidiophores and conidia of Ochroconis gallopava.<br />
MIC µg/mL MIC µg/mL MIC µg/mL<br />
Antifungal Antifungal<br />
Range Range Range<br />
Amphotericin B 0.03-2 Itraconazole 0.03-0.5 Voriconazole 0.03-1<br />
Very limited data, antifungal susceptibility testing of individual strains is recommended.<br />
McGinnis and Pasarell (1998), Espinel-Ingroff (2001) and WCH in-house data.
Descriptions of Medical Fungi 103<br />
Onychocola canadensis Sigler<br />
Teleomorph: Arachnomyces nodososetosus Sigler & Abbott<br />
Colonies grow slowly and are velvety to lanose, white to yellowish, with a brownish<br />
reverse. Arthroconidia are cylindrical to broadly ellipsoidal, one- or two-celled, hyaline<br />
to subhyaline, 4-16 x 2-5 µm in size, forming long chains. Older cultures may show<br />
broad, brown, rough-walled hyphae. RG-2 organism.<br />
Onychocola canadensis is an uncommon cause of distal and lateral subungual or white<br />
superficial onychomycosis. However, it may sometimes be present in an abnormalappearing<br />
nail as an insignificant finding, not acting as a pathogen.<br />
Key Features: slow growing, white, arthroconidial mould isolated from nails.<br />
For descriptions of species, keys to taxa and additional information see Sigler and<br />
Congly (1990), Sigler et al. (1994), Gupta et al. (1998) and de Hoog et al. (2000).<br />
Culture and arthroconidia of Onychocola canadensis.<br />
10 µm
104<br />
Descriptions of Medical Fungi<br />
Paecilomyces Bain<br />
Colonies are fast growing, powdery or suede-like, gold, green-gold, yellow-brown, lilac<br />
or tan, but never green or blue-green as in Penicillium. Phialides are swollen at their<br />
bases, gradually tapering into a rather long and slender neck, and occur solitarily, in<br />
pairs, as verticils, and in penicillate heads. Long, dry chains of single-celled, hyaline<br />
to dark, smooth or rough, ovoid to fusoid conidia are produced in basipetal succession<br />
from the phialides.<br />
The genus Paecilomyces may be distinguished from the closely related genus Penicillium<br />
by having long slender divergent phialides and colonies that are never typically<br />
green. Paecilomyces species are common environmental moulds and are seldom<br />
associated with human infection. However, some species, P. variotii, P. marquandii<br />
and P. lilacinus are emerging as causative agents of mycotic keratitis and of hyalohyphomycosis<br />
in the immunocompromised patient.<br />
Key Features: long slender divergent phialides and culture pigmentation.<br />
For descriptions of species, keys to taxa and additional information see Samson (1974),<br />
Domsch et al. (1980), McGinnis (1980), Onions et al. (1981), Rippon (1988) and de<br />
Hoog et al. (2000).<br />
a b<br />
Cultures of P. variotii (a) and P. lilacinus (b) showing colony pigmentation.
Descriptions of Medical Fungi 105<br />
Antifungal<br />
Paecilomyces lilacinus (Thom) Samson<br />
Colonies are fast growing, suede-like to floccose, vinaceous to violet-coloured. Conidiophores<br />
are erect 400-600 µm in length, bearing branches with densely clustered<br />
phialides. Conidiophore stipes are 3-4 µm wide, yellow to purple and rough-walled.<br />
Phialides are swollen at their bases, gradually tapering into a slender neck. Conidia<br />
are ellipsoidal to fusiform, smooth-walled to slightly roughened, hyaline to purple in<br />
mass, 2.5-3.0 x 2-2.2 µm, and are produced in divergent chains. Chlamydospores are<br />
absent. Growth at 38 O C. RG-1 organism.<br />
Key Features: colony pigmentation, phialides with swollen bases, and pigmented and<br />
rough-walled conidiophore stipes, absence of chlamydospores.<br />
10 µm 10 µm<br />
Conidiophores, phialides and conidia of Paecilomyces lilacinus. Note:<br />
rough-walled conidiophore (arrow).<br />
MIC µg/mL<br />
MIC µg/mL<br />
Range MIC90 Antifungal Range MIC90 Amphotericin B 2-16 8 Posaconazole 0.06-2 0.5 (2)<br />
Itraconazole 0.5-16 16 Voriconazole 0.06-4 0.25 (2)<br />
Limited data, antifungal susceptibility testing of individual strains is recommended.<br />
Espinel-Ingroff et al. (2001), Espinel-Ingroff (2001, 2003), Gonzales et al. (2005), and<br />
WCH in-house data.
106<br />
Descriptions of Medical Fungi<br />
Paecilomyces variotii Bain<br />
Colonies are fast growing, powdery to suede-like, funiculose or tufted, and yellowbrown<br />
or sand-coloured. Conidiophores bearing dense, verticillately arranged branches<br />
bearing phialides. Phialides are cylindrical or ellipsoidal, tapering abruptly into a<br />
rather long and cylindrical neck. Conidia are subspherical, ellipsoidal to fusiform, hyaline<br />
to yellow, smooth-walled, 3-5 x 2-4 µm and are produced in long divergent chains.<br />
Chlamydospores are usually present, singly or in short chains, brown, subspherical to<br />
pyriform, 4-8 µm in diameter, thick-walled to slightly verrucose. RG-2 organism.<br />
Key Features: yellow-brown colony pigmentation, cylindrical phialides, and presence<br />
of chlamydospores.<br />
10 µm 5 µm 10 µm<br />
Conidiophores, phialides, conidia and terminal chlamydospores of P. variotii.<br />
Antifungal<br />
MIC µg/mL<br />
MIC µg/mL<br />
Range MIC90 Antifungal Range MIC90 Amphotericin B 0.06-1 1 Posaconazole 0.03-0.5 0.5<br />
Itraconazole 0.03-8 0.5 Voriconazole 0.03-2 0.5<br />
Limited data, antifungal susceptibility testing of individual strains is recommended.<br />
Espinel-Ingroff et al. (2001), Espinel-Ingroff (2003) and WCH in-house data.
Descriptions of Medical Fungi 107<br />
Paracoccidioides brasiliensis (Splendore) Almeida<br />
Colonies (SDA) at 25 O C are slow growing and variable in morphology. Colonies may<br />
be flat, wrinkled and folded, glabrous, suede-like or downy in texture, white to brownish<br />
with a tan or brown reverse. Microscopically, a variety of conidia may be seen, including<br />
pyriform microconidia, chlamydospores and arthroconidia. However, none of these<br />
are characteristic of the species, and most strains may grow for long periods of time<br />
without the production of conidia.<br />
On BHI blood agar at 37 O C, the mycelium converts to the yeast phase and colonies<br />
are white to tan, moist and glabrous and become wrinkled, folded and heaped. Microscopically,<br />
numerous large, 20-60 μm, round, narrow base budding yeast cells are<br />
present. Single and multiple budding occurs, the latter are thick-walled cells that form<br />
the classical “steering wheel” or “mickey mouse” structures that are diagnostic for this<br />
fungus, especially in methenamine silver stained tissue sections.<br />
WARNING: RG-3 Organism. Cultures of Paracoccidioides brasiliensis may represent<br />
a biohazard to laboratory personnel and should be handled with extreme caution in an<br />
appropriate pathogen handling cabinet. P. brasiliensis is geographically restricted to<br />
areas of South and Central America (Rippon, 1988).<br />
Key Features: clinical history, tissue pathology, culture identification with conversion<br />
to yeast phase at 37 O C.<br />
For descriptions of species, keys to taxa and additional information see McGinnis<br />
(1980), Chandler et al. (1980), Rippon (1988) and de Hoog et al. (2000).<br />
20 µm<br />
20 µm<br />
Multiple, narrow base budding yeast cells “steering wheels” of P. brasiliensis.<br />
Antifungal<br />
MIC µg/mL<br />
Range MIC90 Antifungal<br />
MIC µg/mL<br />
Range MIC90 Amphotericin B 0.03-4 0.25 Itraconazole 0.03-1 0.06<br />
Fluconazole 0.125-64 na Voriconazole 0.03-2 na<br />
Limited data available. Espinel-Ingroff et al. (2001), Espinel-Ingroff (2001) and<br />
Sabatelli et al. (2006) (na = not available).
108<br />
Descriptions of Medical Fungi<br />
Penicillium Link: Fries<br />
Colonies are usually fast growing, in shades of green, sometimes white, mostly consisting<br />
of a dense felt of conidiophores. Microscopically, chains of single-celled conidia<br />
are produced in basipetal succession from a specialised conidiogenous cell called<br />
a phialide. The term basocatenate is often used to describe such chains of conidia<br />
where the youngest conidium is at the basal or proximal end of the chain. In Penicillium,<br />
phialides may be produced singly in groups or from branched metulae, giving a<br />
brush-like appearance (a penicillus). The penicillus may contain both branches and<br />
metulae (penultimate branches which bear a whorl of phialides). All cells between the<br />
metulae and the stipes of the conidiophores are referred to as branches. The branching<br />
pattern may be either simple (non-branched or monoverticillate), one-stage branched<br />
(biverticillate-symmetrical), two-stage branched (biverticillate-asymmetrical) or three-<br />
to more-staged branched. Conidiophores are hyaline, smooth or rough-walled. Phialides<br />
are usually flask-shaped, consisting of a cylindrical basal part and a distinct neck,<br />
or lanceolate (more or less with a narrow basal part tapering to a somewhat pointed<br />
apex). Conidia are in long dry chains, divergent or in columns, are globose, ellipsoidal,<br />
cylindrical or fusiform, hyaline or greenish, smooth or rough-walled. Sclerotia are<br />
produced by some species. RG-1 organisms, with the exception of P. marneffei which<br />
is an RG-3 organism.<br />
For identification, isolates are usually inoculated at three points on Czapek Dox agar<br />
and 2% Malt extract agar and incubated at 25 O C. Most species sporulate within 7<br />
days. Microscopic mounts are best made using a cellotape flag or a slide culture<br />
preparation mounted in lactophenol cotton blue. A drop of alcohol is usually needed to<br />
remove bubbles and excess conidia (see Samson et al., 1995).<br />
Key Features: hyphomycete, flask-shaped phialides arranged in groups from branched<br />
metulae forming a penicillus.<br />
metulae<br />
branches<br />
phialides<br />
a b c d<br />
Morphological structures and types of conidiophore branching in Penicillium.<br />
(a) simple; (b) one-stage branched; (c) two-stage branched; (d) three-stage<br />
branched (see Samson et al. 1995).
Descriptions of Medical Fungi 109<br />
Penicillium Link:Fries<br />
Many species of Penicillium are common contaminants on various substrates and are<br />
known as potential mycotoxin producers. Correct identification is therefore important<br />
when studying possible Penicillium contamination of food. In some species odour and<br />
exudate production will help to recognise the taxa, but it should be pointed out that<br />
inhalation of conidia and volatiles may affect health. Human pathogenic species are<br />
rare, however opportunistic infections leading to mycotic keratitis, otomycosis and endocarditis<br />
(following insertion of valve prosthesis) have been reported (see Samson et<br />
al., 1995 and Rippon, 1988).<br />
For descriptions of species, keys to taxa and additional information see Raper and<br />
Thom (1949), Pitt (1979), Domsch et al. (1980), McGinnis (1980), Onions et al. (1981),<br />
Ramirez (1982), Samson et al. (1995) and de Hoog et al. (2000).<br />
20 µm 20 µm<br />
Conidiophores of P. verrucosum var. cyclopium showing two-stage branching. Simple<br />
conidiophore of P. cheresanum showing long chains of single-celled conidia.<br />
Antifungal<br />
MIC µg/mL<br />
MIC µg/mL<br />
Range MIC90 Antifungal Range MIC90 Amphotericin B 0.125-2 1-2 Posaconazole 0.03-2 0.25-1<br />
Itraconazole 0.03-2 0.5-2 Voriconazole 0.03->8 0.5-2<br />
Limited data, antifungal susceptibility testing of individual strains is recommended.<br />
Pfaller et al. (2002), Diekema et al. (2003), Espinel-Ingroff (2003) and WCH in-house<br />
data.
110<br />
Descriptions of Medical Fungi<br />
Penicillium marneffei Segretain<br />
Colonies (SDA) at 25 O C are fast growing, suede-like to downy, white with yellowishgreen<br />
conidial heads. Colonies become greyish-pink to brown with age and produce<br />
a diffusible brownish-red to wine-red pigment. Conidiophores are hyaline, smoothwalled<br />
and bear terminal verticils of 3-5 metulae, each bearing 3-7 phialides. Conidia<br />
are globose to subglobose, 2 to 3 µm in diameter, smooth-walled and are produced in<br />
basipetal succession from the phialides.<br />
On brain heart infusion (BHI) blood agar incubated at 37 O C, colonies are rough, glabrous,<br />
tan-coloured and yeast-like. Microscopically, yeast cells are spherical to ellipsoidal,<br />
2-6 µm in diameter, and divide by fission rather than budding. Numerous short<br />
hyphal elements are also present.<br />
WARNING: RG-3 organism. Cultures of Penicillium marneffei may represent a biohazard<br />
to laboratory personnel and should be handled with caution in an appropriate<br />
pathogen handling cabinet. P. marneffei exhibits thermal dimorphism and is endemic<br />
in Southeast Asia and the southern region of China.<br />
Tissue sections show small, oval to elliptical yeast-like cells, 3 µm in diameter, either<br />
packed within histiocytes or scattered through the tissue. Occasional, large, elongated<br />
sausage-shaped cells, up to 8 µm long, with distinctive septa may be present.<br />
5 µm<br />
15 µm 5 µm<br />
Colony, a giemsa stained touch smear showing typical septate yeast-like cells<br />
(arrow), phialides and conidia of Penicillium marneffei.
Descriptions of Medical Fungi 111<br />
Phaeoacremonium parasiticum (Ajello et al.) W. Gams et al.<br />
Synonym: Phialophora parasiticum Ajello, Gerog & Wang<br />
Cultures are usually slow growing, suede-like with radial furrows, initially whitish-grey<br />
becoming olivaceous-grey with age. Hyphae hyaline, later becoming brown and some<br />
becoming rough-walled. Phialides are brown, thick-walled, slender, acular to cylindrical<br />
slightly tapering towards the tip, 15-50 μm long, often proliferating, with small, funnel-shaped<br />
collarettes. Conidia, often in balls, are hyaline, thin-walled, cylindrical to<br />
sausage-shaped, 3-6 x 1-2 μm, later inflating (de Hoog et al. 2000). RG-2 organism.<br />
P. parasiticum is a plant pathogen but it has also been reported from cases of<br />
subcutaneous infection, arthritis, mycetoma, endocarditis and mycotic keratitis.<br />
For descriptions of species and additional information see de Hoog et al. (2000).<br />
Antifungal<br />
20 µm<br />
10 µm<br />
Colony, phialides and conidia of Phaeoacremonium parasiticum.<br />
MIC µg/mL MIC µg/mL MIC µg/mL<br />
Antifungal Antifungal<br />
Range Range Range<br />
Amphotericin B 0.06-16 Itraconazole 0.06-32 Voriconazole 0.06-2<br />
Very limited data, antifungal susceptibility testing of individual strains is recommended.<br />
McGinnis and Pasarell (1998) and WCH in-house data.
112<br />
Descriptions of Medical Fungi<br />
Phialophora Medlar<br />
Colonies are usually slow growing, grey to olivaceous-black, often becoming brown<br />
with age. Microscopically, members of the genus Phialophora produce clusters of<br />
single-celled conidia in basipetal succession from characteristic flask-shaped or cylindrical<br />
phialides which have distinctive collarettes. Conidia are hyaline to olivaceous<br />
brown, smooth-walled, ovoid to cylindrical or allantoid, and usually aggregate in slimy<br />
heads at the apices of the phialides, which may be solitary, or in a brush-like arrangement.<br />
The genus Phialophora contains more than 40 species, most are saprophytes commonly<br />
found in soil or on decaying wood. However, several species have been documented<br />
as causing either chromoblastomycosis (P. verrucosa) or phaeohyphomycosis<br />
(P. verrucosa and P. richardsiae).<br />
Phialophora richardsiae (Nannf.) Conant<br />
Colonies grow rapidly, and are powdery to woolly or tufted, greyish-brown with a greybrown<br />
to olivaceous-black reverse. Two conidial types are produced; (1) hyaline conidia<br />
which are allantoid or cylindrical, 3-6 x 1.5-2.5 μm in size, formed on inconspicuous,<br />
peg-like phialides on thin-walled hyphae; and (2) brown, thick-walled conidia which are<br />
spherical to sub-spherical, 2.5-3.5 x 2-3 μm, formed on dark brown, slender, tapering<br />
phialides with flaring collarettes. RG-2 organism.<br />
Phialophora richardsiae is a soft rot fungus of wood and is an uncommon cause of<br />
human infection. However, cases of subcutaneous phaeohyphomycosis have been<br />
reported.<br />
Antifungal<br />
10 µm<br />
10 µm<br />
Phialides of P. richardsiae producing 2 types of conidia. (1) hyaline conidia, formed on<br />
inconspicuous, peg-like phialides on thin-walled hyphae; and (2) brown, thick-walled<br />
conidia formed on dark brown, slender, tapering phialides with flaring collarettes.<br />
MIC µg/mL MIC µg/mL MIC µg/mL<br />
Antifungal Antifungal<br />
Range Range Range<br />
Amphotericin B 0.125-1 Itraconazole 0.03-2 Voriconazole 0.125-2<br />
Very limited data, antifungal susceptibility testing of individual strains is recommended.<br />
McGinnis and Pasarell (1998) and WCH in-house data.
Descriptions of Medical Fungi 113<br />
Phialophora verrucosa Medlar<br />
Colonies (SDA) are slow growing, initially dome-shaped, later becoming flat, suedelike<br />
and olivaceous to black in colour. Phialides are flask-shaped or elliptical with distinctive<br />
funnel-shaped, darkly pigmented collarettes. Conidia are ellipsoidal, smoothwalled,<br />
hyaline, mostly 3.0-5.0 x 1.5-3.0 μm, and aggregate in slimy heads at the<br />
apices of the phialide. RG-2 organism.<br />
Phialophora verrucosa is a well documented causative agent of chromoblastomycosis,<br />
and mycetoma. It produces characteristic flask-shaped phialides with distinctive funnel-shaped,<br />
darkly pigmented collarettes.<br />
For descriptions of species, keys to taxa and additional information see Ellis (1971),<br />
McGinnis (1978), Domsch et al. (1980), McGinnis (1980) and de Hoog et al. (2000).<br />
Antifungal<br />
20 µm<br />
20 µm<br />
Phialides and conidia of Phialophora verrucosa.<br />
MIC µg/mL MIC µg/mL MIC µg/mL<br />
Antifungal Antifungal<br />
Range Range Range<br />
Amphotericin B 0.03-4 Itraconazole 0.03-0.06 Voriconazole 0.03-0.5<br />
Very limited data, antifungal susceptibility testing of individual strains is recommended.<br />
McGinnis and Pasarell (1998) and WCH in-house data.
114<br />
Descriptions of Medical Fungi<br />
Phoma Saccardo<br />
Colonies are spreading, greyish-brown, powdery or suede-like and produce large,<br />
globose, membranous to leathery, darkly pigmented, ostiolate pycnidia. Conidia are<br />
produced in abundance within the pycnidia on narrow thread-like phialides, which are<br />
hardly differentiated from the inner pycnidial wall cells. Conidia are globose to cylindrical,<br />
one-celled, hyaline, and are usually extruded in slimy masses from the apical<br />
ostiole. RG-1 organism.<br />
Members of the genus Phoma have a world-wide distribution and are ubiquitous in<br />
nature, with over 2000 species having been described from soil, as saprophytes on<br />
various plants, and as pathogens to plants and humans.<br />
Key Features: coelomycete, ostiolate pycnidia producing masses of slimy, hyaline,<br />
single-celled conidia.<br />
For descriptions of species, keys to taxa and additional information see Punithalingam<br />
(1979), McGinnis (1980), Sutton (1980), Rippon (1988), Montel et al. (1991), Samson<br />
et al. (1995) and de Hoog et al. (2000).<br />
20 µm<br />
Pycnidia of Phoma.
Descriptions of Medical Fungi 115<br />
Pithomyces Berkeley and Broome<br />
Colonies are fast growing, dark grey to black, suede-like to downy and produce darkly<br />
pigmented, multicellular conidia formed on small peg-like branches of the vegetative<br />
hyphae. Conidia are broadly elliptical, pyriform, oblong, and are commonly echinulate<br />
or verrucose.<br />
The genus Pithomyces contains about 15 species commonly found from a very wide<br />
range of plant material, also from air, soil, hay, sawn timber and ceiling plaster. However,<br />
one species, Pithomyces chartarum is often involved with facial eczema of sheep.<br />
Pithomyces chartarum (Berk. & M.A. Curtis) M.B. Ellis<br />
Colonies are fast growing, suede-like to downy and black. Conidiophores are pale olive,<br />
smooth or verrucose, 2.5-10 x 2-3.5 µm. Conidiogenous cells integrated, intercalary<br />
or terminal, indeterminate, with 1-2 loci of similar width in the conidiogenous cells.<br />
Conidia muriform, medium to dark brown, echinulate to verrucose, 3 (-4)-euseptate,<br />
slightly constricted at the septa, with one or both median cells divided by longitudinal<br />
septa, thick-walled, broadly ellipsoidal, apex obtuse, base truncate and characteristically<br />
with part of the conidiogenous cell remaining attached as a small pedicel, 18-29<br />
x 10-17 µm. RG-1 organism.<br />
Key Features: dematiaceous hyphomycete with multi-celled conidia produced on<br />
small peg-like branches of the vegetative hyphae.<br />
For descriptions of species, keys to taxa and additional information see Ellis (1971 and<br />
1976), Domsch et al. (1980) and Rippon (1988).<br />
15 µm<br />
Conidiophores and conidia of Pithomyces chartarum.
116<br />
Descriptions of Medical Fungi<br />
Prototheca Kruger<br />
Prototheca species are achlorophyllous algae with phylogenetic affinities to the genus<br />
Chlorella. Colonies are smooth, moist, white to cream and yeast-like. Cultures are<br />
sensitive to cycloheximide (actidione) and optimal growth occurs at 25 O C to 30 O C.<br />
Mycelium and conidia are absent. Vegetative cells are globose to ovoid, hyaline, varying<br />
in size from approximately 8-20 µm, and have a relatively thick and highly refractile<br />
wall. No budding cells are present; reproduction is by the development of large sporangia<br />
(theca) which contain from 2-20 or more small sporangiospores (endospores or<br />
autospores) which are asexually produced by nuclear division and cleavage of the cytoplasm<br />
(Kaplan, 1977, McGinnis, 1980, Rippon, 1988, Pore, 1985). RG-1 organism.<br />
Key Features: achlorophyllous algae reproducing by sporangia (theca) and sporangiospores<br />
(autospores). The genus Prototheca contains four species which can be<br />
differentiated by assimilation tests and morphological criteria as outlined below. The<br />
API 20C yeast identification strip may be used for species identification. So far only P.<br />
wickerhamii and P. zopfii have been involved in human or animal infections.<br />
P. wickerhamii P. zopfii P. stagnora P. moriformis<br />
Growth at 37 O C + + - -<br />
Glucose + + + +<br />
Trehalose + - - -<br />
L-propanol - + +/- +<br />
Acetate (pH5) - + +/- +<br />
Galactose + - + -<br />
Capsule - - + +<br />
Antifungal<br />
5 µm<br />
Thecae and autospores of Prototheca wickerhamii.<br />
MIC µg/mL MIC µg/mL MIC µg/mL<br />
Antifungal<br />
Antifungal<br />
Range Range Range<br />
Amphotericin B 0.25-0.5 Voriconazole 0.25 Posaconazole 0.25<br />
WCH in-house data only.
Descriptions of Medical Fungi 117<br />
Ramichloridium Stahel ex de Hoog<br />
Colonies are rapid growing, smooth, farinose or velvety, brown or olivaceous-green,<br />
often with orange or yellow soluble pigments. Conidiophores are erect, brown, apically<br />
with small denticles on which conidia are produced in sympodial succession. Conidia<br />
are one-celled, hyaline to pale brown.<br />
Ramichloridium contains about 25 species that are usually associated with forest litter<br />
and rotting wood, however the genus contains two species of medical interest; R.<br />
mackenziei and R. schulzeri.<br />
Ramichloridium schulzeri (Sacc.) de Hoog<br />
Colonies growing moderately rapidly, consisting of a rather compact, flat, submerged<br />
mycelium, pale orange, locally with some powdery, brownish aerial mycelium; reverse<br />
pink to orange. Conidiophores are erect, straight, unbranched, thick-walled, reddishbrown,<br />
up to 250 µm high, gradually becoming paler towards the apex, of variable<br />
length, elongating sympodially during conidiogenesis, with scattered, pimple-shaped<br />
conidium bearing denticles which have unpigmented scars. Conidia are subhyaline,<br />
smooth-walled or slightly rough-walled, ellipsoidal, obovoidal or fusiform, 6.5-10.0 x 3-<br />
4 µm, usually with an acuminate base and unpigmented scars. RG-1 organism.<br />
For descriptions of species, keys to taxa and additional information see de Hoog (1977),<br />
Rippon et al. (1985) and de Hoog et al. (2000).<br />
10 µm<br />
20 µm<br />
Conidiophores showing sympodial development of conidia of R. schulzeri.
118<br />
Descriptions of Medical Fungi<br />
Rhinocladiella Nannfeldt<br />
Colonies are restricted, velvety, lanose or nearly smooth, grey to olivaceous-brown.<br />
Hyphae pale olivaceous. Conidiophores are slightly differentiated, sub-erect, usually<br />
branched, pale to dark brown. Conidiogenous cells are intercalary or free, cylindrical,<br />
in the apical part with conidium bearing denticles with unpigmented scars. Conidia are<br />
hyaline to subhyaline, one-celled and smooth-walled. Budding cells and an accompanying<br />
Exophiala state may be present.<br />
Rhinocladiella contains 6-8 species, with two species of medical interest; R. atrovirens<br />
and R. aquaspersa.<br />
Rhinocladiella atrovirens Nannfeldt<br />
Colonies are restricted, velvety or lanose, olivaceous, often slightly mucoid at the centre;<br />
reverse dark olivaceous green to blackish. Conidiophores are short, brown, thickwalled.<br />
Conidiogenous cells are cylindrical, intercalary or free, 9-19 x 1.6-2.2 µm;<br />
denticulate rachis up to 15 µm long, with crowded, flat or butt-shaped, unpigmented<br />
conidial denticles. Conidia are hyaline, thin- and smooth-walled, short-cylindrical,<br />
with truncate basal scars, 3.7-5.5 x 1.2-1.8 µm. Budding cells, if present, are hyaline,<br />
thin-walled, broadly ellipsoidal, 3.0-4.3 x 1.7-2.5 µm. Germinating cells are inflated,<br />
spherical to subspherical, 4.5-6.0 µm. An annellidic Exophiala synanamorph may be<br />
present. RG-1 organism.<br />
For descriptions of species, keys to taxa and additional information see de Hoog (1977,<br />
1983), Schell et al. (1983) and de Hoog et al. (2000).<br />
Antifungal<br />
10 µm 10 µm 10 µm<br />
Culture, conidiophores showing a terminal denticulate rachis, conidia and budding<br />
yeast cells of Rhinocladiella atrovirens.<br />
MIC µg/mL MIC µg/mL MIC µg/mL<br />
Antifungal Antifungal<br />
Range Range Range<br />
Amphotericin B 0.03-0.25 Itraconazole 0.03-0.06 Voriconazole 0.03-0.5<br />
Very limited data, antifungal susceptibility testing of individual strains is recommended.<br />
McGinnis and Pasarell (1998), Espinel-Ingroff et al. (2001) and WCH in-house data.
Descriptions of Medical Fungi 119<br />
The genus Rhizomucor is distinguished from Mucor by the presence of stolons and<br />
poorly developed rhizoids at the base of the sporangiophores and by the thermophilic<br />
nature of its 3 species: R. miehei, R. pusillus and R. tauricus. All 3 of these species<br />
are potential human and animal pathogens and were originally classified in the genus<br />
Mucor. Rhizomucor variabilis as described by de Hoog et al. (2000) is not thermophilic<br />
and is probably a degenerate culture of Mucor hiemalis (Voigt et al., 1999). Rhizomucor<br />
pusillus is cosmopolitan and both R. miehei and R. pusillus have been reported as<br />
pathogens to humans and animals, the latter to a greater extent.<br />
For descriptions of species, keys to taxa and additional information see Cooney and<br />
Emerson (1964), Schipper (1978), Domsch et al. (1980), McGinnis (1980), Ellis and<br />
Keane (1981), Scholer et al. (1983), Hoog et al. (2000), Schipper and Staplers (2003)<br />
and Ellis (2005b).<br />
Remember, identification of most zygomycetes is based primarily on the morphology<br />
of the sporangia; i.e. arrangement and number of sporangiospores, shape, colour,<br />
presence or absence of columellae and apophyses, as well as the arrangement of the<br />
sporangiophores and the presence or absence of rhizoids. Growth temperature tests<br />
can also be especially helpful in identifying and differentiating members of the genera<br />
Rhizomucor, Rhizopus and Absidia.<br />
Rhizomucor miehei (Cooney and Emerson) Schipper<br />
Synonym: Mucor miehei Lindt<br />
This species has been reported as a rare cause of bovine mastitis (Scholer et al. 1983)<br />
and is similar in most respects to R. pusillus. However, all strains are homothallic<br />
forming numerous zygospores, which are reddish-brown to blackish-brown, globose to<br />
slightly compressed, up to 50 µm in diameter, with stellate warts and equal suspensor<br />
cells. Colony colour is a dirty grey rather than brown, and sporangia have spiny walls,<br />
are up to 50-60 µm in diameter, with columellae rarely larger than 30 µm in diameter.<br />
Growth is stimulated by thiamine, with no assimilation of sucrose and maximum temperature<br />
of growth is 54–58 O C. RG-1 organism.<br />
Key Features: growth at 45 O C, the formation of numerous zygospores, a dirty grey<br />
culture colour and a partial growth requirement for thiamine.<br />
Synonym: Mucor pusillus Lindt<br />
Rhizomucor Lucet & Costantin<br />
Rhizomucor pusillus (Lindt) Schipper<br />
This species is a rare human pathogen. It has been reported from cases of pulmonary,<br />
disseminated and cutaneous types of infection. It is more often associated with animal<br />
disease, especially bovine abortion. Rhizomucor pusillus has a world-wide distribution<br />
and is commonly associated with compost heaps.
120<br />
Descriptions of Medical Fungi<br />
Rhizomucor pusillus (Lindt) Schipper<br />
This thermophilic zygomycete is readily recognizable by its characteristic compact, low<br />
growing (2-3 mm high), grey to greyish brown-coloured mycelium and by the development<br />
of typical sympodially branched, hyaline to yellow-brown sporangiophores (8-15<br />
μm in diameter), always with a septum below the sporangium. Sporangia are globose<br />
(40-60 µm in diameter), each possessing an oval or pear-shaped columella (20-30<br />
µm), often with a collarette. Sporangiospores are hyaline, smooth-walled, globose to<br />
subglobose, occasionally oval (3-5 µm), and are often mixed with crystalline remnants<br />
of the sporangial wall. Chlamydospores are absent. Zygospores are rough-walled,<br />
reddish brown to black, 45-65 mm in diameter and may be produced throughout the<br />
aerial hyphae in matings between compatible isolates. Temperature growth range:<br />
minimum 20-27 O C; optimum 35-55 O C; maximum 55-60 O C. There is positive assimilation<br />
of sucrose and no thiamine dependence. RG-2 organism.<br />
Key Features: zygomycete, growth at 45 O C (thermophilic), poorly developed stolons<br />
and rhizoids, branching sporangiophores with a septum below the sporangium, darkcoloured<br />
sporangia without apophyses and smooth-walled globose to subglobose<br />
sporangiospores.<br />
15 µm 20 µm<br />
Sporangiophores, collumellae and primitive rhizoids of R. pusillus.<br />
Antifungal<br />
MIC µg/mL<br />
MIC µg/mL<br />
Antifungal<br />
Range Range<br />
Fluconazole >64 Amphotericin B 0.06-0.25<br />
Itraconazole 0.03-0.25 Flucytosine >256<br />
Posaconazole 0.06-0.25 Voriconazole 2-16<br />
Very limited data, antifungal susceptibility testing of individual strains is<br />
recommended. Dannaoui et al. (2003), Singh et al. (2005) and WCH inhouse<br />
data.
Descriptions of Medical Fungi 121<br />
The genus Rhizopus is characterised by the presence of stolons and pigmented rhizoids,<br />
the formation of sporangiophores, singly or in groups from nodes directly above<br />
the rhizoids, and apophysate, columellate, multispored, generally globose sporangia.<br />
After spore release the apophyses and columella often collapse to form an umbrellalike<br />
structure. Sporangiospores are globose to ovoid, one-celled, hyaline to brown<br />
and striate in many species. Colonies are fast growing and cover an agar surface with<br />
a dense cottony growth that is at first white becoming grey or yellowish brown with<br />
sporulation.<br />
Antifungal<br />
Rhizopus Ehrenberg ex Corda.<br />
MIC µg/mL<br />
MIC µg/mL<br />
Range MIC<br />
Antifungal<br />
Range MIC 90 90<br />
Fluconazole >64 >64 Amphotericin B 0.03-4 2<br />
Itraconazole 0.25-8 4 Flucytosine >256 >256<br />
Posaconazole 0.03-8 2 Voriconazole 4->64 >64<br />
Very limited data, antifungal susceptibility testing of individual strains is recommended.<br />
Sun et al. (2002), Dannaoui et al. (2003), Espinel-Ingroff (2001, 2003), Singh et al.<br />
(2005), Sabatelli et al. (2006) and WCH in-house data.<br />
In the past, numerous attempts have been made to clarify the species concepts of<br />
the genus Rhizopus. Recently, 3 excellent revisions with easy to use keys have been<br />
produced by Schipper (1984), Ellis (1985, 1986) and Schipper and Stalpers (2003).<br />
Basically, 3 groups have been recognised: the ‘stolonifer’ group, the ‘oryzae’ group and<br />
the ‘microsporus’ group. The G-C values of the 3 groups have been defined by Frye<br />
and Reinhardt (1993), and temperature growth studies at 30 O C, 36 O C and 45 O C are<br />
characteristic for each of the groups.<br />
The ‘stolonifer’ group has sporangia up to 275 µm in diameter and grows at 30 O C, but<br />
has a maximum growth temperature of 36 O C. Species in this group include R. sexualis<br />
and R. stolonifer. The latter has been unconvincingly implicated in human infection<br />
(Ferry and Abedi 1983), although with a maximum growth temperature of only 32 O C its<br />
pathogenicity is thus questionable.<br />
The ‘oryzae’ group has been reduced to a single species that is able to grow at 40 O C<br />
but not at 45 O C, and has sporangia not exceeding 240 µm in diameter. There is no<br />
doubt that R. oryzae and R. arrhizus are synonymous, the contentious issue being<br />
which species name to use. The taxonomic treatment of Schipper and Stalpers (2003)<br />
will be used in this book; however, the synonym R. arrhizus is commonly used in the<br />
medical literature. Rhizopus oryzae is an important human pathogen.<br />
The ‘microsporus’ group has simple rhizoids, and smaller sporangia up to 100 µm in<br />
diameter and grows at both 40 and 45 O C. This group contains 4 species: R. homothallicus,<br />
R. azygosporus, R. schipperae and R. microsporus with the later subdivided into<br />
3 varieties, namely R. microsporus var. microsporus, R. microsporus var. oligosporus<br />
and R. microsporus var. rhizopodiformis. All are thermophilic and R. microsporus is a<br />
well-recognised pathogen of humans and animals.
122<br />
Descriptions of Medical Fungi<br />
Rhizopus Ehrenberg ex Corda.<br />
Differentiation of pathogenic Rhizopus microsporus group isolates.<br />
Species Growth<br />
at 45O Growth<br />
C at 50O Main species characteristics<br />
C<br />
R. azygosporus Good No Abundant azygospores<br />
R. microsporus var. Good No Sporangiospores angular to ellipsoidal<br />
microsporus<br />
and distinctly striate, up to 5–6 µm diam<br />
R. microsporus var. Restricted No Sporangiospores globose, up to<br />
oligosporus<br />
9 µm diameter or more, heterogeneous<br />
R. microsporus var. Good Good Sporangiospores globose rarely over 5<br />
rhizopodiformis<br />
µm in diameter minutely spinulose<br />
R. schipperae Good No Abundant chlamydospores and<br />
restricted sporulation<br />
For descriptions of species, keys to taxa and additional information, see Domsch et al.<br />
(1980), McGinnis (1980), Onions et al. (1981), Scholer et al. (1983), Schipper (1984),<br />
Schipper and Stalpers (1984, 2003), Ellis (1985, 1986), Rippon (1988), Kwon-Chung<br />
and Bennett (1992), Samson et al. (1995); Hoog et al. (2000) and Ellis (2005b).<br />
Rhizopus azygosporus Yuan & Jong<br />
Rhizopus azygosporus is closely related to R. microsporus (Yuan and Jong 1984) and<br />
has been reported as the causative agent of 3 fatal cases of gastrointestinal infection<br />
in premature babies (Woodward et al. 1992, Schipper et al. 1996). Previously, this fungus<br />
was only known from its type culture, which has been isolated from tempeh, a solid<br />
fermented soybean food from Indonesia (Yuan and Jong 1984). Colonies are whitish<br />
to grey-black, producing pale-brown simple rhizoids. Sporangiophores are brownish,<br />
up to 350 µm high and 6-14 µm wide. Sporangia are greyish-black, spherical and<br />
50-100 µm in diameter. Columellae are subglobose to globose. Sporangiospores<br />
are ovoid to ellipsoidal 4-5 to 6-7 µm in diameter with faint striations. Azygospores<br />
are pale to dark-brown, spherical to subglobose, 30–70 µm in diameter, with coarse<br />
conical projections. All strains produce abundant azygospores in unmated isolates as<br />
a species characteristic. There is good growth at 45 O C with a maximum of 46-48 O C.<br />
RG-2 organism.<br />
Rhizopus microsporus var. microsporus<br />
Rhizopus microsporus var. microsporus is a rare cause of human infection (Kerr et al.<br />
1988, Kwon-Chung and Bennett, 1992). Colonies are pale brownish-grey producing<br />
simple rhizoids. Sporangiophores are brownish, up to 400 µm high and 10 µm wide,<br />
but most are smaller and are produced in pairs. Sporangia are greyish-black, spherical,<br />
up to 80 µm in diameter. Columellae are subglobose to globose to conical. Sporangiospores<br />
are angular to broadly ellipsoidal to lemon-shaped, quite equal in size,<br />
up to 5-6 µm in diameter and are distinctly striate. Zygospores, formed by crosses of<br />
compatible mating strains, are dark red–brown, spherical, up to 100 µm in diameter,<br />
with stellate projections and unequal suspensor cells. There is good growth at 45 O C,<br />
with a maximum of 46–48 O C. RG-2 organism.
Descriptions of Medical Fungi 123<br />
Rhizopus microsporus var. oligosporus (Saito) Schipper & Stalpers<br />
Rhizopus microsporus var. oligosporus is a rare cause of human zygomycosis (Tintelnot<br />
and Nitsche 1989). Colonies are pale yellowish-brown to grey and sporulation is<br />
often poor. Rhizoids are subhyaline and simple. Sporangiophores are brownish, up to<br />
300 µm high and 15 µm wide, with 1-3 produced together. Sporangia are black, spherical,<br />
up to 100 µm in diameter. Columellae are subglobose to somewhat conical. Sporangiospores<br />
are subglobose to globose, up to 9 µm in diameter, almost smooth, with<br />
larger spores often irregular in shape. Chlamydospores are abundant, hyaline, single<br />
or in chains, spherical, ellipsoidal or cylindrical, 7-35 µm in diameter. Zygospores are<br />
not known. There is growth at 45 O C with a maximum of 46–48 O C. RG-2 organism.<br />
Rhizopus microsporus var. rhizopodiformis (Cohn) Schipper & Stalpers<br />
Rhizopus microsporus var. rhizopodiformis is the second most frequently isolated zygomycete,<br />
accounting for between 10% and 15% of reported human cases (Scholer<br />
et al. 1983; Kwon-Chung and Bennett 1992). Colonies are dark greyish-brown, up to<br />
10 mm high with simple rhizoids. Sporangiophores are brownish, up to 500 µm high<br />
and 8 µm wide, with 1-4 produced together. Sporangia are bluish to greyish-black,<br />
spherical and up to 100 µm in diameter. Columellae are pyriform comprising 80% of<br />
the sporangium. Sporangiospores are subglobose to globose, quite equal in size, up<br />
to 6 µm in diameter and minutely spinulose. Zygospores, when formed by crosses of<br />
compatible mating strains, are reddish-brown, spherical, up to 100 µm in diameter, with<br />
stellate projections and unequal suspensor cells. There is good growth at 45 O C with a<br />
maximum of 50–52 O C. RG-2 organism.<br />
30 µm<br />
Sporangia showing sporangiophores, columellae, sporangiospores<br />
and rhizoids of R. microsporus var. oligosporus.
124<br />
Descriptions of Medical Fungi<br />
Rhizopus oryzae Went & Prinsen Geerligs<br />
Synonym: Rhizopus arrhizus Fischer<br />
Rhizopus oryzae is the most common causative agent of zygomycosis, accounting for<br />
some 60% of the reported culture positive cases, and nearly 90% of the rhinocerebral<br />
form of infection. Colonies are very fast growing, about 5-8 mm high, with some tendency<br />
to collapse, white cottony at first becoming brownish grey to blackish-grey depending<br />
on the amount of sporulation. Sporangiophores up to 1500 µm in length and<br />
18 µm in width, smooth-walled, non-septate, simple or branched, arising from stolons<br />
opposite rhizoids usually in groups of 3 or more. Sporangia are globose, often with a<br />
flattened base, greyish black, powdery in appearance, up to 175 µm in diameter and<br />
many spored. Columellae and apophysis together are globose, subglobose or oval, up<br />
to 130 µm in height and soon collapsing to an umbrella-like form after spore release.<br />
Sporangiospores are angular, subglobose to ellipsoidal, with ridges on the surface,<br />
and up to 8 µm in length. No growth at 45 O C; good growth at 40 O C. RG-2 organism<br />
20 µm<br />
100 µm<br />
Culture, sporangia, sporangiophores and rhizoids of R.oryzae.
Descriptions of Medical Fungi 125<br />
Rhodotorula Harrison<br />
The genus Rhodotorula is characterised by the combination of red or yellow cultures<br />
due to the presence of carotenoid pigments, the inability to assimilate inositol and the<br />
absence of fermentation. The basidiomycetous nature of yeasts is usually indicated<br />
by a positive urease test. The genus Cryptococcus is similar to Rhodotorula both in<br />
production of carotenoid pigments and the presence of capsulated blastoconidia. The<br />
distinctive difference between the two is the assimilation of inositol, which is positive in<br />
Cryptococcus.<br />
Rhodotorula mucilaginosa is a common airborne contaminant of skin, lungs, urine and<br />
faeces. R. mucilaginosa is a known cause of fungal peritonitis in patients on continuous<br />
ambulatory peritoneal dialysis (CAPD). This is usually due to saprophytic colonisation<br />
of catheters or dialysis machinery and removal of the source of contamination<br />
usually leads to clearing of the symptoms.<br />
For descriptions of species, keys to taxa and additional information see McGinnis<br />
(1980), Barnett et al. (1983), Kreger-Van Rij (1984), Rippon (1988), Kurtzman and<br />
Fell (1988) and de Hoog et al. (2000).<br />
Culture of Rhodotorula mucilaginosa.
126<br />
Descriptions of Medical Fungi<br />
Rhodotorula glutinis (Fresenius) Harrison<br />
Culture: Colonies (SDA) are coral red to salmon-coloured or slightly orange, smooth<br />
to wrinkled, highly glossy to semi-glossy. Mucoid to pasty to slightly tough, yeast-like<br />
colonies.<br />
Microscopy: Ovoidal to globose or more elongate budding yeast-like cells or blastoconidia,<br />
2.3-5.0 x 4.0-10.0 µm.<br />
India Ink Preparation: Small capsules present.<br />
Dalmau Plate Culture on Cornmeal and Tween 80 Agar: Budding blastoconidia<br />
only. No pseudohyphae are formed.<br />
Physiological Tests: + Positive, - Negative, v Variable, w Weak, s Slow<br />
Germ Tube - L-Sorbose v L-Arabinose v D-Glucitol v<br />
Fermentation Sucrose + D-Arabinose v α-M-D-glucoside v<br />
Glucose - Maltose + D-Ribose v D-Gluconate +<br />
Galactose - Cellobiose v L-Rhamnose v DL-Lactate v<br />
Sucrose - Trehalose + D-Glucosamine - myo-Inositol -<br />
Maltose - Lactose - N-A-D-glucosamine - 2-K-D-gluconate v<br />
Lactose - Melibiose - Glycerol v D-Glucuronate v<br />
Trehalose - Raffinose v Erythritol - Nitrate -<br />
Assimilation Melezitose + Ribitol v Urease +<br />
Glucose + Soluble Starch - Galactitol v 0.1% Cycloheximide v<br />
Galactose v D-Xylose v D-Mannitol v Growth at 37 O C v<br />
Key Features: germ tube negative yeast and sugar assimilation pattern. Common<br />
saprophyte however cases of fungemia have been reported. RG-1 organism.<br />
Antifungal<br />
MIC µg/mL<br />
MIC µg/mL<br />
Range Antifungal<br />
Range<br />
Fluconazole >64 Amphotericin B 0.06-0.25<br />
Itraconazole 0.5-1 Flucytosine 0.03-0.06<br />
Voriconazole 1-4 Caspofungin 0.25<br />
Very limited data, antifungal susceptibility testing of individual strains is recommended.<br />
WCH in-house data only.
Descriptions of Medical Fungi 127<br />
Synonym: Rhodotorula rubra (Demme) Lodder.<br />
Culture: Colonies (SDA) are coral pink, usually smooth, sometimes reticulate, rugose<br />
or corrugated, moist to mucoid, yeast-like colonies.<br />
Microscopy: Spherical to elongate budding yeast-like cells or blastoconidia, 2.5-6.5 x<br />
6.5-14.0 µm.<br />
India Ink Preparation: Negative - No capsules present.<br />
Dalmau Plate Culture on Cornmeal and Tween 80 Agar: Budding blastoconidia<br />
only. No pseudohyphae are formed.<br />
Key Features: germ tube negative yeast and sugar assimilation pattern. Common<br />
saprophyte however cases of peritonitis and fungemia have been reported. RG-1<br />
organism.<br />
Antifungal<br />
Rhodotorula mucilaginosa (Jorgensen) Harrison<br />
Physiological Tests: + Positive, - Negative, v Variable, w Weak, s Slow<br />
Germ Tube - L-Sorbose v L-Arabinose v D-Glucitol v<br />
Fermentation Sucrose + D-Arabinose v α-M-D-glucoside v<br />
Glucose - Maltose v D-Ribose v D-Gluconate +<br />
Galactose - Cellobiose v L-Rhamnose v DL-Lactate v<br />
Sucrose - Trehalose + D-Glucosamine v myo-Inositol -<br />
Maltose - Lactose - N-A-D-glucosamine - 2-K-D-gluconate v<br />
Lactose - Melibiose - Glycerol v D-Glucuronate -<br />
Trehalose - Raffinose + Erythritol v Nitrate -<br />
Assimilation Melezitose v Ribitol v Urease +<br />
Glucose + Soluble Starch - Galactitol v 0.1% Cycloheximide -<br />
Galactose v D-Xylose + D-Mannitol v Growth at 40 O C +<br />
MIC µg/mL<br />
MIC µg/mL<br />
Range MIC90 Antifungal Range MIC90 Fluconazole 0.5->64 >64 Amphotericin B 0.03-1 0.5<br />
Itraconazole 0.25-4 2 Flucytosine 0.03-0.25 0.25<br />
Voriconazole 0.25-4 2 Caspofungin 16 >16<br />
Very limited data, antifungal susceptibility testing of individual strains is recommended.<br />
Espinel-Ingroff et al. (2001), Espinel-Ingroff (2003), Cuenca-Estrella et al. (2006) and<br />
WCH in-house data.
128<br />
Descriptions of Medical Fungi<br />
Saccharomyces cerevisiae Meyen ex Hansen<br />
The genus Saccharomyces is characterised by strong fermentation of at least glucose<br />
and the presence of rather large globose to ellipsoidal cells with multilateral budding.<br />
Pseudohyphae can be formed, but never true hyphae. Ascospores are globose to ellipsoidal,<br />
with a smooth wall, usually one to four per ascus. Lactose and nitrate are<br />
not utilised. The species S. cerevisiae, commonly known as Baker’s yeast, is the most<br />
important representative.<br />
Culture: Colonies (SDA) are white to cream, smooth, glabrous yeast-like colonies.<br />
Microscopy: Large globose to ellipsoidal budding yeast-like cells or blastoconidia,<br />
3.0-10.0 x 4.5-21.0 µm.<br />
India Ink Preparation: Negative - No capsules present.<br />
Dalmau Plate Culture on Cornmeal and Tween 80 Agar: Usually budding blastoconidia<br />
only, however pseudohyphae may be formed rarely.<br />
Physiological Tests: + Positive, - Negative, v Variable, w Weak, s Slow<br />
Germ Tube - L-Sorbose - L-Arabinose - D-Glucitol -<br />
Fermentation Sucrose + D-Arabinose - α-M-D-glucoside v<br />
Glucose + Maltose + D-Ribose - D-Gluconate -<br />
Galactose v Cellobiose - L-Rhamnose - DL-Lactate v<br />
Sucrose + Trehalose + D-Glucosamine - myo-Inositol -<br />
Maltose v Lactose - N-A-D-glucosamine - 2-K-D-gluconate -<br />
Lactose - Melibiose v Glycerol - D-Glucuronate -<br />
Trehalose - Raffinose + Erythritol - Nitrate -<br />
Assimilation Melezitose v Ribitol - Urease -<br />
Glucose + Soluble Starch - Galactitol - 0.1% Cycloheximide -<br />
Galactose v D-Xylose - D-Mannitol - Growth at 37 O C v<br />
Key Features: germ tube negative yeast and sugar assimilation pattern. Common<br />
food and environmental saprophyte. RG-1 organism.<br />
For descriptions of species, keys to taxa and additional information see McGinnis<br />
(1980), Barnett et al. (1983), Kreger-Van Rij (1984), Rippon (1988), Kurtzman and<br />
Fell (1988) and de Hoog et al. (2000).<br />
Antifungal<br />
MIC µg/mL<br />
MIC µg/mL<br />
Range MIC90 Antifungal Range MIC90 Fluconazole 0.125-16 8 Amphotericin B 0.06-2 1<br />
Itraconazole 0.03-4 0.5 Flucytosine 0.03-0.5 0.25<br />
Voriconazole 0.06-0.25 0.125 Caspofungin 1 1<br />
Very limited data, antifungal susceptibility testing of individual strains is recommended.<br />
Espinel-Ingroff et al. (2001), Espinel-Ingroff (2003), Cuenca-Estrella et al. (2006)<br />
and WCH in-house data.
Descriptions of Medical Fungi 129<br />
Saksenaea vasiformis Saksena<br />
The genus Saksenaea is characterised by the formation of flask-shaped sporangia<br />
with columellae and simple, darkly pigmented rhizoids. Saksenaea vasiformis is the<br />
only known species and appears to have a world-wide distribution in association with<br />
soil. It is an emerging human pathogen (Holland, 1997) that is most often associated<br />
with cutaneous or subcutaneous lesions after trauma. Colonies are fast growing,<br />
downy, white with no reverse pigment made up of broad, non-septate hyphae typical of<br />
a zygomycetous fungus. Sporangia are typically flask-shaped with a distinct spherical<br />
venter and long-neck, arising singly or in pairs from dichotomously branched, darkly<br />
pigmented rhizoids. Collumellae are prominent and dome-shaped. Sporangiospores<br />
are small, oblong, 1-2 x 3-4 µm, and are discharged through the neck following the dissolution<br />
of an apical mucilaginous plug. RG-2 organism.<br />
Key Features: zygomycete, unique flask-shaped sporangia, failure to sporulate on<br />
primary isolation media.<br />
Laboratory identification of this fungus may be difficult or delayed because of the<br />
mould’s failure to sporulate on the primary isolation media or on subsequent subculture<br />
onto potato dextrose agar. Sporulation may be stimulated by the use of nutrient deficient<br />
media, like cornmeal-glucose-sucrose-yeast extract agar, Czapek Dox agar, or<br />
by using the agar block method described by Ellis and Ajello (1982), Ellis and Kaminski<br />
(1985) and Padhye and Ajello (1988).<br />
For descriptions of species, keys to taxa and additional information see Saksena<br />
(1953), Ellis and Hesseltine (1966), Ajello et al. (1976), Ellis and Ajello (1982), Ellis<br />
and Kaminski (1985), Pritchard et al. (1986), Padhye et al. (1988), Padhye and Ajello<br />
(1988), Goldschmied-Reouven et al. (1989), de Hoog et al. (2000) and Ellis (2005b).<br />
Antifungal<br />
The agar block method to induce<br />
sporulation of Saksenaea vasiformis<br />
and Apophysomyces elegans.<br />
A small block of agar is cut from a well<br />
established culture grown on PDA and<br />
is placed in the centre of petri dish<br />
containing 1% agar in distilled water.<br />
After 21 days at 26 O C look for sporangium<br />
formation at the periphery of the<br />
petri dish.<br />
MIC µg/mL<br />
MIC µg/mL<br />
Antifungal<br />
Range Range<br />
Fluconazole >64 Amphotericin B 0.125-2<br />
Itraconazole 0.015-0.3 Flucytosine >256<br />
Posaconazole 0.015-0.25 Voriconazole 0.5-4<br />
Very limited data, poor sporulation, antifungal susceptibility testing of individual strains<br />
is recommended. Sun et al. (2002) and WCH in-house data.
130<br />
Descriptions of Medical Fungi<br />
Saksenaea vasiformis Saksena<br />
15 µm<br />
Sporangium of Saksenaea vasiformis.
Descriptions of Medical Fungi 131<br />
Scedosporium apiospermum/aurantiacum Complex<br />
Recent genetic studies have shown Scedosporium apiospermum to be a species complex<br />
and two species of medical importance have now been recognised: S. apiospermum<br />
and S. aurantiacum (Gilgado et al. 2005).<br />
Scedosporium apiospermum (Saccardo) Castellani and Chalmers<br />
Colonies are fast growing, greyish-white, suede-like to downy with a greyish-black reverse.<br />
Numerous single-celled, pale-brown, broadly clavate to ovoid conidia, 4-9 x 6-<br />
10 mm, rounded above with truncate bases are observed. Conidia are borne singly or<br />
in small groups on elongate, simple or branched conidiophores or laterally on hyphae.<br />
Conidial development can be described as annellidic, although the annellations (ringlike<br />
scars left at the apex of an annellide after conidial secession) are extremely difficult<br />
to see. Optimum temperature for growth is 30-37 O C. RG-2 organism.<br />
Ascocarp formation may be stimulated on cornmeal agar or other nutrient deficient<br />
media, however it should be noted that many isolates may fail to produce cleistothecia.<br />
Cleistothecia (non-ostiolate ascocarps) are yellow-brown to black, spherical, are mostly<br />
submerged in the agar and are composed of irregularly interwoven brown hyphae.<br />
When crushed cleistothecia release numerous, faintly brown, ellipsoidal ascospores,<br />
4-5 x 7- 9 µm in size. A Graphium synanamorph may also be present.<br />
The teleomorph is currently referred to as Pseudallescheria boydii, however as all<br />
species of Pseudallescheria have Scedosporium anamorphs, it is presumptive to use<br />
the teleomorph name to describe this fungus without seeing cleistothecia (ascocarps).<br />
Until the taxonomy of Pseudallescheria is resolved, it is recommended that laboratories<br />
use the anamorphic name Scedosporium apiospermum when describing this fungus.<br />
Scedosporium aurantiacum Gilgado et al.<br />
All isolates produce a light yellow diffusible pigment on PDA after a few days incubation.<br />
Conidiogenous cells and conidia are similar in shape and size to S. apiospermum,<br />
and the two can best be distinguished by genetic analysis. Conidiogenous cells arising<br />
from undifferentiated hyphae are cylindrical to slightly flask-shaped, producing slimy<br />
heads of one-celled , smooth-walled, subhyaline, obovoid or sub-cylindrical conidia.<br />
5-14 x 2-5 um. Erect synnemata (a Graphium synanamorph) may be present in some<br />
isolates, but the teleomorph is unknown. Optimum temperature for growth 37-40 O C,<br />
max 45 O C. RG-2 organism.<br />
S. apiospermum and S. aurantiacum appear to be common soil fungi capable of causing<br />
a spectrum of diseases similar in terms of variety and severity to those caused by<br />
Aspergillus collectively referred to as Pseudallescheriasis. The vast majority of infections<br />
are mycetomas, the remainder include infections of the eye, ear, central nervous<br />
system, internal organs and more commonly the lungs.<br />
For descriptions of species, keys to taxa and additional information see McGinnis<br />
(1980), Domsch et al. (1980), McGinnis et al. (1982), Campbell and Smith (1982), Rippon<br />
(1988), de Hoog et al. (2000) and Gilgado et al. (2005).
132<br />
Descriptions of Medical Fungi<br />
Scedosporium apiospermum (Saccardo) Castellani and Chalmers<br />
Antifungal<br />
Culture and a cleistothecium of Pseudallescheria boydii.<br />
20 µm<br />
20 µm<br />
Conidiophores (annellides) and conidia of Scedosporium apiospermum.<br />
MIC µg/mL<br />
MIC µg/mL<br />
Range MIC90 Antifungal Range MIC90 Itraconazole 0.06-4 2 Amphotericin B 1-16 16<br />
Voriconazole 0.03-1 0.5 Posaconazole 0.5-2 1<br />
Good data available. McGinnis and Pasarell (1998), Espinel-Ingroff (2001, 2003),<br />
Espinel-Ingroff et al. (2001) and Cuenca-Estrella et al. (2006). MIC 90 s from the<br />
Australian Scedosporium Study.
Descriptions of Medical Fungi 133<br />
Scedosporium aurantiacum Gilgado et al.<br />
Culture reverse (PDA) of S. apiospermum (left) and S. aurantiacum (right) showing<br />
the production of a light yellow diffusible pigment that is typical of S. aurantiacum.<br />
Antifungal<br />
20 µm<br />
Conidiophores (annellides) and conidia of Scedosporium aurantiacum.<br />
MIC µg/mL<br />
MIC µg/mL<br />
Range MIC90 Antifungal Range MIC90 Itraconazole 0.25-2 1 Amphotericin B 2-16 16<br />
Voriconazole 0.03-0.5 0.25 Posaconazole 0.125-1 0.5<br />
Good data available. Australian Scedosporium Study.
134<br />
Descriptions of Medical Fungi<br />
Scedosporium prolificans (Hennebert & Desai) Gueho & de Hoog<br />
Synonym: Scedosporium inflatum Malloch & Salkin<br />
Colonies are rapid growing, flat, spreading, olive-grey to black and have a suede-like<br />
to downy surface texture. Conidia are borne in small groups on distinctive basally<br />
swollen, flask-shaped annellides, which occur singly or in clusters along the vegetative<br />
hyphae. Conidia are single-celled, hyaline to pale-brown, ovoid to pyriform, 2-5 x 3-13<br />
µm (average 3.4 x 5.3 µm), and have smooth thin walls. RG-2 organism.<br />
Key Features: dematiaceous hyphomycete with initial black pasty colony, basally<br />
swollen (inflated) annellides and no growth on media containing cycloheximide<br />
(actidione).<br />
For descriptions of species, keys to taxa and additional information see Malloch and<br />
Salkin (1984), Salkin et al. (1988), Rippon (1988), Wilson et al. (1990), Gueho and de<br />
Hoog (1991) and de Hoog et al. (2000).<br />
Antifungal<br />
20 µm<br />
Conidiophores (annellides) and conidia of Scedosporium prolificans.<br />
MIC µg/mL<br />
MIC µg/mL<br />
Range MIC90 Antifungal Range MIC90 Itraconazole 1-32 >8 Amphotericin B 1-16 >8<br />
Voriconazole 0.5-32 >8 Posaconazole >8 >8<br />
Good data available. McGinnis and Pasarell (1998), Espinel-Ingroff (2001, 2003),<br />
Espinel-Ingroff et al. (2001), Sabatelli et al. (2006), Cuenca-Estrella et al. (2006) and<br />
the Australian Scedosporium Study.
Descriptions of Medical Fungi 135<br />
Schizophyllum commune Fries<br />
Colonies on 2% malt extract agar are spreading, woolly, whitish to pale greyish-brown,<br />
soon forming macroscopically visible fruiting bodies. Although some isolates may take<br />
up to 12 weeks to form fruiting bodies. Fruit bodies are sessile, kidney-shaped, lobed<br />
with split gills on the lower side. Hyphae are hyaline, wide and have clamp connections<br />
(although many primary clinical isolates are monokaryotic and will therefore not<br />
produce clamp connections). Basidia bear 4 basidiospores on erect sterigmata. Basidiospores<br />
hyaline, smooth-walled, elongate with lateral scar at lower end, 6-7 x 2-3<br />
µm.<br />
Shizophyllum is a common bracket fungus on rotten wood, and is an occasional human<br />
pathogen, principally associated with sinusitis, allergic bronchopulmonary mycosis<br />
and as a contaminant from respiratory specimens. RG-1 organism.<br />
Note: many clinical isolates of S. commune are monokaryotic and therefore do not<br />
show clamp connections, therefore any white, rapidly growing, sterile isolate showing<br />
good growth at 37 O C with tolerance to benomyl, susceptibility to cycloheximide, and a<br />
pronounced odour should be suspected of being S. commune (Sigler et al., 1995).<br />
For descriptions of species, keys to taxa and additional information see McGinnis<br />
(1980), Rippon (1988), Sigler et al. (1995) and de Hoog et al. (2000).<br />
Basidiocarps of Schizophyllum commune on malt extract agar.
136<br />
Descriptions of Medical Fungi<br />
Scopulariopsis Bain<br />
Colonies are fast growing, varying in colour from white, cream, grey, buff to brown,<br />
black, but are predominantly light brown. Microscopic morphology shows chains of<br />
single-celled conidia produced in basipetal succession from by a specialised conidiogenous<br />
cell called an annellide. Once again, the term basocatenate can be used<br />
to describe such chains of conidia where the youngest conidium is at the basal end of<br />
the chain. In Scopulariopsis, annellides may be solitary, in groups, or organised into<br />
a distinct penicillus. Conidia are globose to pyriform, usually truncate, with a rounded<br />
distal portion, smooth to rough, and hyaline to brown in colour.<br />
Most members of the genus Scopulariopsis are soil fungi, however a few, in particular<br />
S. brevicaulis, have been reported as causative agents of onychomycosis and hyalohyphomycosis.<br />
RG-2 for species isolated from humans.<br />
Key Features: hyphomycete, conidia often shaped like light globes, basocatenate<br />
arising from annellides.<br />
For descriptions of species, keys to taxa and additional information see Morton and<br />
Smith (1963), Domsch et al. (1980), McGinnis (1980), Rippon (1988), Samson et al.<br />
(1995) and de Hoog et al. (2000).<br />
Antifungal<br />
10 µm<br />
Conidiophores (annellides) and conidia of Scopulariopsis brevicaulis.<br />
MIC µg/mL MIC µg/mL MIC µg/mL<br />
Antifungal Antifungal<br />
Range Range Range<br />
Amphotericin B 2-16 Itraconazole 32 Voriconazole 2-8<br />
Very limited data, antifungal susceptibility testing of individual strains is recommended.<br />
McGinnis and Pasarell (1998) and WCH in-house data.
Descriptions of Medical Fungi 137<br />
Sepedonium Link ex Greville<br />
Colonies are moderately fast growing, usually white to golden yellow, suede-like to<br />
downy, becoming fluffy with age. Conidiophores are hyaline and non-specialised, resembling<br />
short branches of the vegetative hyphae. Conidia are terminal, solitary, or<br />
in clusters, one-celled, globose to ovoid, 7 to 17 µm, hyaline to amber, smooth to verrucose<br />
and usually with a thick wall.<br />
The microscopic morphology of Sepedonium isolates resembles that of Histoplasma<br />
capsulatum. Therefore, positive identification of the latter, requires conversion of the<br />
mould form to the yeast phase by growth at 37 O C on enriched media or by exoantigen<br />
test. RG-1 organism.<br />
Key Features: hyphomycete, producing large, thick-walled, one-celled, verrucose,<br />
globose, terminal macroconidia from non-specialised conidiophores, resembling Histoplasma<br />
capsulatum.<br />
For descriptions of species, keys to taxa and additional information see McGinnis<br />
(1980) and Rippon (1988).<br />
Conidia of Sepedonium.<br />
15 µm
138<br />
Descriptions of Medical Fungi<br />
Sporothrix schenckii Hektoen & Perkins<br />
Colonies (SDA) at 25 O C, are slow growing, moist and glabrous, with a wrinkled and<br />
folded surface. Some strains may produce short aerial hyphae and pigmentation may<br />
vary from white to cream to black. Conidiophores arise at right angles from thin septate<br />
hyphae and are usually solitary, erect and tapered toward the apex. Conidia are<br />
formed in clusters on tiny denticles by sympodial proliferation at the apex of the conidiophore,<br />
their arrangement often suggestive of a flower. As the culture ages, conidia<br />
are subsequently formed singly along the sides of both conidiophores and undifferentiated<br />
hyphae. Conidia are ovoid or elongated, 3-6 x 2-3 µm, hyaline, one-celled and<br />
smooth-walled. In some isolates, solitary, darkly-pigmented, thick-walled, one-celled,<br />
obovate to angular conidia may also be observed along the hyphae.<br />
On brain heart infusion agar containing blood at 37 O C, colonies are glabrous, white to<br />
greyish-yellow and yeast-like consisting of spherical or oval budding yeast cells.<br />
Sporothrix schenckii is a dimorphic fungus and has a world-wide distribution, particularly<br />
in tropical and temperate regions. It is commonly found in soil and on decaying<br />
vegetation and is a well known pathogen of humans and animals. Sporotrichosis is<br />
primarily a chronic mycotic infection of the cutaneous or subcutaneous tissues and adjacent<br />
lymphatics characterised by nodular lesions which may suppurate and ulcerate.<br />
Infections are caused by the traumatic implantation of the fungus into the skin, or very<br />
rarely, by inhalation into the lungs. Secondary spread to articular surfaces, bone and<br />
muscle is not infrequent, and the infection may also occasionally involve the central<br />
nervous system, lungs or genitourinary tract. RG-2 organism.<br />
Key Features: hyphomycete characterised by thermal dimorphism and clusters of<br />
ovoid, denticulate conidia produced sympodially on short conidiophores.<br />
For descriptions of species, keys to taxa and additional information see McGinnis<br />
(1980), Domsch et al. (1980), de Hoog et al. (1985), Rippon (1988) and de Hoog et al.<br />
(2000).<br />
10 µm<br />
Periodic Acid-Schiff (PAS) stained tissue section showing budding<br />
yeast-like cells of S. schenckii.
Descriptions of Medical Fungi 139<br />
Antifungal<br />
Sporothrix schenckii Hektoen & Perkins<br />
10 µm<br />
Culture on SDA at 25 O C and budding yeast cells in BHI at 37 O C.<br />
10 µm<br />
Conidiophores and conidia of Sporothrix schenckii on SDA at 25 O C.<br />
MIC µg/mL<br />
MIC µg/mL<br />
Range MIC90 Antifungal Range MIC90 Fluconazole 32->64 >64 Amphotericin B 0.06->16 >16<br />
Itraconazole 0.03->16 0.5 (4) Flucytosine 4->64 >64<br />
Posaconazole 0.125-4 2 Caspofungin 1->8 nd<br />
Voriconazole 0.125->16 4 (16) Anidulafungin 0.25->8 nd<br />
Limited data, antifungal susceptibility testing of individual strains is recommended.<br />
McGinnis et al. (2001), Espinel-Ingroff et al. (2001), Espinel-Ingroff (2003), Gonzales<br />
et al. (2005) and Alvarado-Ramirez and Torres-Rodriguez (2007). (nd = not done).
140<br />
Descriptions of Medical Fungi<br />
Stemphylium Wallroth<br />
Colonies are rapid growing, brown to olivaceous-black or greyish and suede-like to<br />
floccose. Microscopically, solitary, darkly pigmented, terminal, multicellular conidia<br />
(dictyoconidia) are formed on a distinctive conidiophore with a darker terminal swelling.<br />
Note: the conidiophore proliferates percurrently through the scar where the terminal<br />
conidium (poroconidium) was formed. Conidia are pale to mid-brown, oblong,<br />
rounded at the ends, ellipsoidal, obclavate or subspherical and are smooth or in part<br />
verrucose. Stemphylium should not be confused with Ulocladium which produces similar<br />
dictyoconidia from a sympodial conidiophore, not from a percurrent conidiogenous<br />
cell as in Stemphylium. RG-1 organism.<br />
Key Features: dematiaceous hyphomycete producing darkly pigmented, dictyoconidia<br />
from the swollen end of a percurrent conidiophore.<br />
For descriptions of species, keys to taxa and additional information see Ellis (1971 and<br />
1976), Rippon (1988) and de Hoog et al. (2000).<br />
20 µm<br />
Conidiophores and conidia of Stemphylium.
Descriptions of Medical Fungi 141<br />
Syncephalastrum Schröter<br />
The genus Syncephalastrum is characterised by the formation of cylindrical merosporangia<br />
on a terminal swelling of the sporangiophore. Sporangiospores are arranged<br />
in a single row within the merosporangia. Syncephalastrum racemosum is the type<br />
species of the genus and a potential human pathogen; however, well-documented<br />
cases are lacking. It is found mainly from soil and dung in tropical and subtropical regions.<br />
It can also be a difficult laboratory aerial contaminant. The sporangiophore and<br />
merosporangia of Syncephalastrum species may also be mistaken for an Aspergillus<br />
species, if the isolate is not looked at carefully.<br />
Colonies are very fast growing, cottony to fluffy, white to light grey, becoming dark<br />
grey with the development of sporangia. Sporangiophores are erect, stolon-like, often<br />
producing adventitious rhizoids, and show sympodial branching (racemose branching)<br />
producing curved lateral branches. The main stalk and branches form terminal, globose<br />
to ovoid vesicles which bear finger-like merosporangia directly over their entire<br />
surface. At maturity, merosporangia are thin-walled, evanescent and contain 5-10(18)<br />
globose to ovoid, smooth-walled sporangiospores (merospores). Optimum growth<br />
temperature 20-40 O C. RG-2 organism.<br />
Key Features: zygomycete producing sympodially branching sporangiophores with<br />
terminal vesicles bearing merosporangia.<br />
For descriptions of species, keys to taxa and additional information see Domsch et al.<br />
(1980), McGinnis (1980), Onions et al. (1981), Rippon (1988), Samson et al. (1995),<br />
Hoog et al. (2000) and Ellis (2005b).<br />
30 µm<br />
10 µm<br />
Terminal vesicle, merosporangia and merospores of S. racemosum.
142<br />
Descriptions of Medical Fungi<br />
Trichoderma Persoon ex Grey<br />
Colonies are fast growing, at first white and downy, later developing yellowish-green<br />
to deep green compact tufts, often only in small areas or in concentric ring-like zones<br />
on the agar surface. Conidiophores are repeatedly branched, irregularly verticillate,<br />
bearing clusters of divergent, often irregularly bent, flask-shaped phialides. Conidia<br />
are mostly green, sometimes hyaline, with smooth or rough walls and are formed in<br />
slimy conidial heads (gloiospora) clustered at the tips of the phialides.<br />
Trichoderma is a very common genus especially in soil and decaying wood. Gliocladium<br />
(with strongly convergent phialides) and Verticillium (with straight and moderately<br />
divergent phialides) are closely related genera. Trichoderma is an RG-1 organism.<br />
Key Features: hyphomycete with repeatedly branched conidiophores bearing clusters<br />
of divergent, flask-shaped phialides.<br />
For descriptions of species, keys to taxa and additional information see Domsch et al.<br />
(1980), McGinnis (1980), Rippon (1988), Samson et al. (1995), de Hoog et al. (2000).<br />
Antifungal<br />
20 µm<br />
Phialides and conidia of Trichoderma harzianum.<br />
MIC µg/mL MIC µg/mL MIC µg/mL<br />
Antifungal Antifungal<br />
Range Range Range<br />
Amphotericin B 0.5-2 Itraconazole 2-16 Voriconazole 0.25-2<br />
Very limited data, antifungal susceptibility testing of individual strains is recommended.<br />
Espinel-Ingroff (2001) and WCH in-house data.
Descriptions of Medical Fungi 143<br />
Trichophyton Malmsten<br />
The genus Trichophyton is characterised by the development of both smooth-walled<br />
macro- and microconidia. Macroconidia are mostly borne laterally directly on the hyphae<br />
or on short pedicels, and are thin- or thick-walled, clavate to fusiform, and range<br />
from 4-8 x 8-50 mm in size. Macroconidia are few or absent in many species. Microconidia<br />
are spherical, pyriform to clavate or of irregular shape and range from 2-3 x 2-4<br />
mm in size. The presence of microconidia distinguishes this genus from Epidermophyton<br />
and the smooth-walled, mostly sessile macroconidia separate it from Microsporum.<br />
Twenty species have been recognised, however only the more common species are<br />
included in these descriptions.<br />
In practice, two groups may be recognised on direct microscopy:<br />
1. Those species that usually produce microconidia, macroconidia may or may not be<br />
present i.e. T. rubrum, T. interdigitale, T. mentagrophytes, T. equinum, T. erinacei,<br />
T. tonsurans, T. terrestre and to a lesser extent T. verrucosum, which may produce<br />
conidia on some media; and<br />
2. Those species that usually do not produce conidia. Chlamydospores or other<br />
hyphal structures may be present, but microscopy is generally non-diagnostic; i.e.<br />
T. verrucosum, T. violaceum, T. concentricum, T. schoenleinii and T. soudanense.<br />
Many laboratories seem to have difficulty in distinguishing between species of Trichophyton,<br />
especially isolates of T. rubrum, T. interdigitale, T. mentagrophytes and T.<br />
tonsurans. Basically, the laboratories which consistently identify these fungi correctly<br />
do more work and use additional media and/or confirmatory tests. However, it must<br />
be stressed that no one single test is infallible, dermatophyte species are very variable<br />
organisms and many characteristics either overlap or are inconsistent.<br />
The Mycology Unit at the Adelaide Women’s and Children’s Hospital uses a dermatophyte<br />
identification scheme, devised by the late Geraldine Kaminski, comprising 6<br />
different media to help identify and differentiate the various species and strains of<br />
Trichophyton. The media in this scheme are Littman Oxgall agar, Lactritmel agar,<br />
Sabouraud’s agar with 5% NaCl, 1% Peptone agar, Trichophyton agar No. 1, and hydrolysis<br />
of urea (see appendix for details).<br />
Note: species concepts in dermatophytes are currently in a state of flux. Recent molecular<br />
studies have shown that many species appear to be clonal and that there is<br />
little correlation between “genetic” and “phenotypic” species (Graser et al. 2006). The<br />
descriptions and species concepts provided in this publication are based on traditional<br />
morphological criteria which may not correspond to molecular identification results.<br />
For description of species, keys to taxa and additional information see Rebell and<br />
Taplin (1970), Ajello (1972), Vanbreusegham et al. (1978), Rippon (1988), McGinnis<br />
(1980), Domsch et al. (1980), Kane et al. (1997) and de Hoog et al. (2000).<br />
Antifungal<br />
MIC µg/mL<br />
MIC µg/mL<br />
Range MIC90 Antifungal Range MIC90 Griseofulvin 0.06-4 1-2 Amphotericin B 0.03-16 0.5-1<br />
Itraconazole 0.01-8 0.25-0.5 Fluconazole 0.06->64 32<br />
Terbinafine 0.01-16 0.06 Voriconazole 0.007-8 0.25<br />
Fernandez-Torres et al. (2001), Sabatelli et al. (2006), Santos and Hamdan (2006).
144<br />
Descriptions of Medical Fungi<br />
Trichophyton ajelloi (Vanbreuseghem) Ajello<br />
Teleomorph: Arthroderma uncinatum Dawson and Gentles<br />
Colonies are usually flat, powdery, cream to tan to orange-tan in colour, with a blackish-purple<br />
submerged fringe and reverse. Macroconidia are numerous, smooth, thickwalled,<br />
elongate, cigar-shaped, 29-65 x 5-10 µm, and multiseptate with up to 9 or 10<br />
septa. Microconidia are usually absent, but when present are ovate to pyriform in<br />
shape. RG-1 organism.<br />
Trichophyton ajelloi is a geophilic fungus with a world-wide distribution which may occur<br />
as a saprophytic contaminant on humans and animals. Infections in man and animals<br />
doubtful. Not known to invade hair in vivo, but produces hair perforations in vitro.<br />
Key Features: culture characteristics, macroconidial morphology, urease positive and<br />
good growth on Sabouraud’s 5% salt agar.<br />
20 µm<br />
Culture and macroconidia of Trichophyton ajelloi.
Descriptions of Medical Fungi 145<br />
Trichophyton concentricum Blanchard<br />
Teleomorph: Arthroderma benhamiae Ajello & Chang.<br />
Colonies (SDA) are slow growing, raised and folded, glabrous becoming suede-like,<br />
mostly white to cream-coloured, but sometimes orange-brown-coloured, often deeply<br />
folded into the agar which may produce splitting of the medium in some cultures. Reverse<br />
is buff to yellow-brown to brown in colour. Cultures consist of broad, muchbranched,<br />
irregular, often segmented, septate hyphae which may have “antler” tips<br />
resembling T. schoenleinii. Chlamydospores are often present in older cultures. Microconidia<br />
and macroconidia are not usually produced, although some isolates will<br />
produce occasional clavate to pyriform microconidia. Note: hyphal segments may<br />
artificially resemble macroconidia. RG-2 organism.<br />
Kaminski’s Dermatophyte Identification Scheme<br />
Littman Oxgall Agar: Small, heaped and folded, blue-grey, suede to glabrous colonies<br />
with no reverse or diffusible pigment.<br />
Lactritmel Agar: Colonies tend to be flatter, dull-white, suede-like, almost glabrous<br />
with a yellow-brown reverse pigment. Microscopic morphology is similar to that described<br />
above, however occasional clavate to pyriform microconidia may be present.<br />
Note: occasional, small, slender, smooth thin-walled macroconidia with 2-3 septa have<br />
been reported on specialised media like lactritmel agar, bean pod agar and hay infusion<br />
agar.<br />
Sabouraud’s Dextrose Agar with 5% NaCl: Small, stunted, heaped and folded,<br />
cream to buff, glabrous colonies with no reverse pigment.<br />
1% Peptone Agar: Flat, white, suede-like colony with a pale yellow-brown reverse.<br />
Hydrolysis of Urea: Negative after 7 days<br />
Vitamin Free Agar (Trichophyton Agar No.1): Growth occurs on vitamin free agar<br />
(T1) but is usually slightly better on media containing thiamine i.e. T3 = T1 + thiamine<br />
and inositol, and T4 = T1 + thiamine. The slight enhancement of growth in the presence<br />
of thiamine helps to distinguish T. concentricum from T. schoenleinii, although<br />
this does not occur in all strains.<br />
Hair Perforation Test: Negative at 28 days.<br />
Trichophyton concentricum is an anthropophilic fungus which causes chronic widespread<br />
non-inflammatory tinea corporis known as tinea imbricata because of the concentric<br />
rings of scaling it produces. It is not known to invade hair. Infections among<br />
Europeans are rare. Distribution is restricted to the Pacific Islands of Oceania, South<br />
East Asia and Central and South America.<br />
Key Features: hyphomycete (dermatophyte), clinical disease, geographical distribution<br />
and culture characteristics.
146<br />
Descriptions of Medical Fungi<br />
Trichophyton concentricum Blanchard<br />
20 µm<br />
T. concentricum on mycobiotic agar showing a typical slow<br />
growing, heaped and folded, glabrous to suede like colony.<br />
Microscopic morphology of T. concentricum showing the formation<br />
of typical “balloon-shaped” chlamydospores. Note: microconidia<br />
and macroconidia are usually not produced.
Descriptions of Medical Fungi 147<br />
Trichophyton equinum (Matruchot & Dassonville) Gedoelst<br />
Teleomorph: Arthroderma vanbreuseghemii Takashio<br />
Colonies (SDA) are usually flat, but some may develop gentle folds or radial grooves,<br />
white to buff in colour, suede-like to downy in texture, and are similar to T. mentagrophytes.<br />
Cultures usually have a deep-yellow submerged fringe and reverse which<br />
later becomes dark red in the centre. Microscopically, abundant microconidia which<br />
may be clavate to pyriform and sessile or spherical and stalked are formed laterally<br />
along the hyphae. Macroconidia are only rarely produced, but when present are clavate,<br />
smooth, thin-walled and of variable size. Occasional nodular organs may be<br />
present and the microconidia often undergo a transformation to produce abundant<br />
chlamydospores in old cultures. RG-2 organism.<br />
Kaminski’s Dermatophyte Identification Scheme<br />
Littman Oxgall Agar: Compact, raised velvety white surface with yellowish reverse<br />
and diffusing yellow pigment.<br />
Lactritmel Agar: Flat spreading, white to cream-coloured, powdery to granular surface<br />
with a central downy papilla, and deep brownish red reverse. Microscopic morphology<br />
as described above for the primary culture.<br />
Sabouraud’s Dextrose Agar with 5% NaCl: An extremely stunted, slow growing dark<br />
brown colony with a few submerged brown hyphae.<br />
1% Peptone Agar: Flat white to cream, suede-like surface with raised white downy<br />
centre and pale yellow reverse.<br />
Hydrolysis of Urea: Positive in 4-5 days.<br />
Nutritional Tests on Trichophyton Agars: Most strains require nicotinic acid (Fig. 1)<br />
for growth except those from Australia and New Zealand, which are autotrophic (Fig.<br />
2). T1 = vitamin free agar, T5 = vitamin free + nicotinic acid agar.<br />
Fig. 1. Fig. 2.<br />
Hair Perforation Test: Negative; but positive for the autotrophicum strains.<br />
Key Features: microscopic morphology, culture characteristics, nicotinic acid requirement<br />
and clinical lesions in horses.
148<br />
Descriptions of Medical Fungi<br />
Trichophyton equinum (Matruchot & Dassonville) Gedoelst<br />
Trichophyton equinum is a zoophilic fungus causing ringworm in horses and rare infections<br />
in humans. It has a world-wide distribution except for the autotrophicum strain<br />
which is restricted to Australia and New Zealand. Invaded hairs show an ectothrix<br />
infection but do not fluoresce under Wood’s ultra-violet light.<br />
20 µm<br />
Culture, microconidia, macroconidia and nodular organs of T. equinum.
Descriptions of Medical Fungi 149<br />
Trichophyton erinacei (Smith & Marples) Quaife<br />
Teleomorph: Arthroderma benhamiae Ajello & Chang.<br />
Colonies (SDA) are white, flat, powdery, sometimes downy to fluffy with a brilliant lemon<br />
yellow reverse. Numerous large clavate microconidia are borne on the sides of<br />
hyphae. Macroconidia are smooth-walled, two- to six-celled, clavate, variable in size,<br />
and may have terminal appendages. Macroconidia are much shorter than those seen<br />
in T. mentagrophytes. RG-2 organism.<br />
Kaminski’s Dermatophyte Identification Scheme<br />
Littman Oxgall Agar: White, downy colony with yellowish-green diffusible pigment.<br />
Lactritmel Agar: White suede-like to powdery colony with brilliant yellow reverse.<br />
Numerous large slender clavate microconidia.<br />
Sabouraud’s Dextrose Agar with 5% NaCl: White folded suede-like to powdery<br />
colony with no reverse pigment.<br />
1% Peptone Agar: White, suede-like to powdery colony with pale yellow reverse.<br />
Hydrolysis of Urea: Negative at 7 days.<br />
Vitamin Free Agar (Trichophyton Agar No.1): Good growth indicating no special<br />
nutritional requirements. Colonies are white suede-like to powdery with no reverse<br />
pigment.<br />
Hair Perforation Test: Positive<br />
Trichophyton erinacei is a zoophilic fungus associated with hedgehogs and the epidermal<br />
mites which they often harbour. Human infections occur most frequently on the<br />
exposed parts of the body, but tinea of the scalp and nails can also occur. Invaded<br />
hairs show an ectothrix infection but do not fluoresce under Wood’s ultra-violet light.<br />
The distribution of this fungus is New Zealand and Europe.<br />
Positive “in vitro” hair perforation test.
150<br />
Descriptions of Medical Fungi<br />
Trichophyton erinacei (Smith & Marples) Quaife<br />
Key Features: culture characteristics, microscopic morphology, geographical<br />
distributions and negative urease test.<br />
20 µm<br />
Culture, microconidia and macroconidia of Trichophyton erinacei.<br />
Trichophyton erinacei is generally distinguished from T. mentagrophytes by (a) its<br />
microscopic morphology showing numerous large slender clavate microconidia borne<br />
on the sides of hyphae and its smooth, thin-walled clavate macroconidia; (b) its brilliant<br />
lemon yellow reverse pigment on plain Sabouraud’s agar and Lactritmel agar; (c) its<br />
lack of reverse pigment on Sabouraud’s salt agar; and (d) its negative hydrolysis of<br />
urea.
Descriptions of Medical Fungi 151<br />
Teleomorph: Arthroderma vanbreuseghemii Takashio<br />
Colonies (SDA) are usually flat, white to cream in colour with a powdery to suede-like<br />
surface and yellowish and pinkish brown reverse pigment, often becoming a darker<br />
red-brown with age. Numerous subspherical to pyriform microconidia, occasional spiral<br />
hyphae and spherical chlamydospores are present, the latter being more abundant<br />
in older cultures. Occasional slender, clavate, smooth-walled, multiseptate macroconidia<br />
are also present in some cultures. RG-2 organism.<br />
Kaminski’s Dermatophyte Identification Scheme<br />
Littman Oxgall Agar: raised white downy colony with no reverse pigment.<br />
Lactritmel Agar: Macroscopic and microscopic features as described for the primary<br />
culture.<br />
Sabouraud’s Dextrose Agar with 5% NaCl: Heaped and folded, buff-coloured suedelike<br />
surface with a dark reddish-brown submerged fringe and brown reverse.<br />
1% Peptone Agar: Flat, white to cream, suede-like surface with raised white downy<br />
centre. No reverse pigment.<br />
Hydrolysis of Urea: Positive within 5 days.<br />
Vitamin Free Agar (Trichophyton Agar No.1): Good growth indicating no special<br />
nutritional requirements, flat cream powdery surface with central downy tuft. Reverse<br />
pale pinkish-brown.<br />
Hair Perforation Test: Positive.<br />
Trichophyton interdigitale Priestley<br />
Key Features: culture characteristics, microscopic morphology and in vitro perforation<br />
of human hair.<br />
Trichophyton interdigitale can be distinguished from T. rubrum and T. mentagrophytes<br />
by (a) its culture characteristics and microscopic morphology on Sabouraud’s dextrose<br />
agar and/or lactritmel agar; (b) its growth and colony morphology on Sabouraud’s salt<br />
agar (colonies of T. interdigitale and T. mentagrophytes unlike T. rubrum, grow very<br />
well on this medium and usually produce a distinctive dark reddish-brown reverse pigment);<br />
(c) a positive urease test (within 7 days), a positive hair perforation test and the<br />
production of a yellow-brown to pinkish-brown reverse pigment on pigment stimulation<br />
media like lactritmel and Trichophyton No.1 agars; and (d) on 1% peptone agar<br />
T. interdigitale has a suede-like to downy surface whereas T. mentagrophytes has a<br />
characteristic granular appearance.<br />
Trichophyton interdigitale is an anthropophilic fungus which is a common cause of<br />
tinea pedis, particularly the vesicular type, tinea corporis, and sometimes superficial<br />
nail plate invasion. It is not known to invade hair in vivo but produces hair perforations<br />
in vitro. Distribution is world-wide.
152<br />
Descriptions of Medical Fungi<br />
20 µm<br />
Trichophyton interdigitale Priestley<br />
20 µm<br />
Culture, microconidia, macroconidia, chlamydospores and spiral hyphae in<br />
Trichophyton interdigitale.
Descriptions of Medical Fungi 153<br />
Trichophyton interdigitale var. nodulare<br />
Supplementary description for Trichophyton interdigitale var. nodulare, a dysgonic variant<br />
of T. interdigitale with distinctive bright yellow to apricot-coloured colonies with a<br />
suede-like to powdery surface and a bright yellow-brown to orange reverse. On primary<br />
isolation, colonies are often glabrous with minimal surface mycelium. Microscopically<br />
characteristic “nodular organs” are observed in the vegetative hyphae. Usually,<br />
no conidia are seen but some isolates, especially with subculture, may produce subspherical<br />
to pyriform microconidia similar to those of T. interdigitale. RG-2 organism.<br />
T. interdigitale var. nodulare is an unusual cause of tinea pedis. It has a world-wide distribution.<br />
It is not known to invade hair in vivo, but produces hair perforations in vitro.<br />
20 µm<br />
Culture and “nodular organs” T. interdigitale var. nodulare.
154<br />
Descriptions of Medical Fungi<br />
Trichophyton mentagrophytes (Robin) Blanchard<br />
Teleomorph: Arthroderma simii Stockdale et al.<br />
Colonies (SDA) are generally flat, white to cream in colour, with a powdery to granular<br />
surface. Some cultures show central folding or develop raised central tufts or pleomorphic<br />
suede-like to downy areas. Reverse pigmentation is usually a yellow-brown to<br />
reddish-brown colour. Numerous single-celled microconidia are formed, often in dense<br />
clusters. Microconidia are hyaline, smooth-walled, and are predominantly spherical to<br />
subspherical in shape, however occasional clavate to pyriform forms may occur. Varying<br />
numbers of spherical chlamydospores, spiral hyphae and smooth, thin-walled, clavate-shaped,<br />
multi-celled macroconidia may also be present. RG-2 organism.<br />
Kaminski’s Dermatophyte Identification Scheme<br />
Littman Oxgall Agar: Raised greyish-white, suede-like to downy colony. Some cultures<br />
may show a diffusible yellow to brown pigment.<br />
Lactritmel Agar: Cultures are flat, white to cream in colour, with a powdery to granular<br />
surface. Some cultures develop a raised central tuft or pleomorphic downy areas. Reverse<br />
pigmentation is yellow-brown to pinkish-brown to red-brown. Microscopic morphology<br />
similar to that described above, with predominantly spherical microconidia,<br />
often forming in dense clusters and varying numbers of spherical chlamydospores,<br />
spiral hyphae and smooth, thin-walled, clavate, multiseptate macroconidia.<br />
Sabouraud’s Dextrose Agar with 5% NaCl: Cultures are heaped and folded, buff to<br />
brown in colour, with a suede-like surface texture and characteristically have a very<br />
dark reddish-brown submerged peripheral fringe and reverse pigmentation.<br />
1% Peptone Agar: Flat, cream-coloured, powdery to granular colony with no reverse<br />
pigment.<br />
Hydrolysis of Urea: Positive within 7 days (usually 3 to 5 days).<br />
Vitamin Free Agar (Trichophyton Agar No.1): Good growth indicating no special<br />
nutritional requirements. Cultures are flat, cream-coloured, with a powdery to suedelike<br />
surface, and have a reddish-brown reverse pigmentation.<br />
Hair Perforation Test: Positive within 14 days.<br />
Key Features: culture characteristics, microscopic morphology and clinical disease<br />
with known animal contacts. T. mentagrophytes can be distinguished from T. interdigitale<br />
by (a) its granular appearance on 1% Peptone agar, (b) its microscopic morphology<br />
of more spherical microconidia and generally greater numbers of macroconidia<br />
and (c) a yellow to brown diffusible pigment is often seen on Littman Oxgall agar.<br />
T. mentagrophytes is the zoophilic form of T. mentagrophytes with a world-wide distribution<br />
and a wide range of animal hosts including mice, guinea-pigs, kangaroos, cats,<br />
horses, sheep and rabbits. Produces inflammatory skin or scalp lesions in humans,<br />
particularly in rural workers. Kerion of the scalp and beard may occur. Invaded hairs<br />
show an ectothrix infection but do not fluoresce under Wood’s ultra-violet light.
Descriptions of Medical Fungi 155<br />
Trichophyton mentagrophytes (Robin) Blanchard<br />
20 µm 20 µm<br />
20 µm<br />
Cultures, microconidia, macroconidia, chlamydospores and spiral hyphae in<br />
Trichophyton mentagrophytes.
156<br />
Descriptions of Medical Fungi<br />
Trichophyton mentagrophytes var. quinckeanum (Zopf) MacLeod & Muende<br />
Colonies (SDA) are flat or slightly raised and folded, white to cream, suede-like in<br />
texture with a pale yellow-brown to pinkish brown reverse. A characteristic pungent<br />
“mousy” odour may be present. Numerous microconidia, predominantly slender clavate<br />
when young, are borne laterally along the sides of hyphae. With age the microconidia<br />
become broader and pyriform, and some subspherical forms are present. Occasional<br />
to moderate numbers of smooth-walled, multiseptate, clavate macroconidia<br />
may be present. RG-2 organism.<br />
Kaminski’s Dermatophyte Identification Scheme<br />
Littman Oxgall Agar: Raised, dome-like bluish-grey, suede-like colony with a narrow<br />
flat, greyish-white, suede-like border. No diffusible or reverse pigment should be<br />
present.<br />
Lactritmel Agar: Flat, white to cream, suede-like to powdery colony with either no<br />
reverse pigment or a pale yellow-brown to pinkish-brown reverse. Numerous slender<br />
clavate to pyriform (depending on age of sub-culture) microconidia and occasional to<br />
moderate numbers of smooth, thin-walled, clavate macroconidia are present.<br />
Sabouraud’s Dextrose Agar with 5% NaCl: Heaped up and much folded white<br />
suede-like colony with very pale yellow-brown reverse. No submerged fringe.<br />
1% Peptone Agar: Raised white suede-like to downy colony with no reverse<br />
pigment.<br />
Hydrolysis of Urea: Positive within 7 days (usually very rapid 2-3 days).<br />
Vitamin Free Agar (Trichophyton Agar No.1): Flat, white to cream, suede-like<br />
colony with either no reverse pigment or a pale yellow-brown reverse. i.e. no special<br />
nutritional requirements.<br />
Hair Perforation Test: Positive in 7 to 10 days.<br />
Key Features: culture characteristics, microscopic morphology, contact with mice,<br />
odour and rapid urease test.<br />
T. mentagrophytes var. quinckeanum may be distinguished from T. mentagrophytes by<br />
(a) its characteristic culture appearance on Littman Oxgall agar (i.e. raised, dome-like,<br />
bluish-grey suede-like colony with a narrow flat, greyish-white, suede-like border and<br />
no diffusible or reverse pigment); and on Sabouraud’s salt agar (typically heaped and<br />
folded white suede-like colony, but with no distinctive dark reddish-brown submerged<br />
fringe and reverse pigment as seen in T. mentagrophytes); (b) microscopic morphology<br />
showing numerous slender clavate with some pyriform microconidia and moderate<br />
numbers of smooth thin-walled, clavate macroconidia; (c) a rapid urease test, usually<br />
within 2 to 3 days; and (d) cultures often have a characteristic pungent “mousy”<br />
odour.
Descriptions of Medical Fungi 157<br />
Trichophyton mentagrophytes var. quinckeanum (Zopf) MacLeod & Muende<br />
Trichophyton mentagrophytes var. quinckeanum causes “mouse favus” on mice, and<br />
this is seen as thick, yellow, saucer-shaped crusted lesions up to 1 cm in diameter<br />
called scutula. Invaded hairs are rarely seen but they may show either ectothrix or<br />
endothrix infection. Infected human hairs do not fluoresce under Wood’s ultra-violet<br />
light, but very occasional hairs from experimental lesions in guinea pigs may show a<br />
pale yellow fluorescence. The geographical distribution of this dermatophyte is difficult<br />
to establish, but it is probably world-wide. It is often associated with mice plagues in<br />
the Australian Wheat Belt.<br />
20 µm<br />
Culture, microconidia and macroconidia of T. mentagrophytes var.<br />
quinckeanum.
158<br />
Descriptions of Medical Fungi<br />
Trichophyton rubrum (Castellani) Semon<br />
Many strains and varieties of T. rubrum have been described and opinion differs between<br />
mycologists as to the exact validity of many of these. For practical purposes we<br />
will distinguish two types: T. rubrum downy type and T. rubrum granular type.<br />
Microscopically, the downy type is characterised by the production of scanty to moderate<br />
numbers of slender clavate microconidia and no macroconidia. It frequently causes<br />
chronic infections of skin and nails. Granulomatous lesions may sometimes occur.<br />
Microscopically, the granular type is characterised by the production of moderate to<br />
abundant numbers of clavate to pyriform microconidia and moderate to abundant numbers<br />
of thin-walled, cigar-shaped macroconidia. The macroconidia may or may not<br />
have terminal appendages.<br />
Trichophyton rubrum granular strain is a frequent cause of tinea corporis in South East<br />
Asia and in Aborigines living in the Northern Territory of Australia. However, since the<br />
Vietnam War, it has been spread throughout the world, especially to those countries<br />
with returning troops or to those receiving refugees, where it has often been described<br />
as a new species. The granular strain of T. rubrum represents the parent strain of T.<br />
rubrum downy type; the latter evolved by establishing a niche in feet (tinea pedis) when<br />
the former was imported into Europe and North America at the beginning of the 20th<br />
century. It should be stressed that intermediate strains between the two types do occur<br />
and that many culture and morphological characteristics overlap.<br />
Trichophyton rubrum typical downy strain<br />
Colonies (SDA) are flat to slightly raised, white to cream, suede-like to downy, with a<br />
yellow-brown to wine-red reverse. Most cultures show scanty to moderate numbers of<br />
slender clavate to pyriform microconidia. Macroconidia are usually absent, however<br />
closterospore-like projections may be present in some mounts. Note: on primary isolation<br />
some cultures may lack reverse pigmentation and fail to produce microconidia.<br />
These will need to be subcultured onto media like Lactritmel agar or potato dextrose<br />
agar which stimulate pigmentation and sporulation. If sporulation still fails subculture<br />
the fungus onto Trichophyton Agar No.1. RG-2 organism.<br />
Culture of Trichophyton rubrum downy strain.
Descriptions of Medical Fungi 159<br />
Trichophyton rubrum (Castellani) Semon<br />
Kaminski’s Dermatophyte Identification Scheme<br />
Littman Oxgall Agar: Raised, greyish-white, suede-like to downy colony with no reverse<br />
pigment. Some cultures may have showed a faint greenish-yellow diffusible<br />
pigment.<br />
Lactritmel Agar: Flat, white, downy colonies with a deep wine-red reverse pigment.<br />
Microscopically, cultures show the typical downy type morphology of pyriform to slender<br />
clavate microconidia.<br />
Sabouraud’s Dextrose Agar with 5% NaCl: Very stunted, white downy colony with a<br />
pale yellow-brown reverse pigment.<br />
1% Peptone Agar: Flat, white to cream, downy colony often with a raised centre. No<br />
reverse pigment produced.<br />
Hydrolysis of Urea: Negative at 7 days.<br />
Vitamin Free Agar (Trichophyton Agar No.1): Good growth indicating no special<br />
vitamin requirements. Colonies are flat, white to cream, suede-like to downy with a<br />
deep wine-red reverse pigment.<br />
Hair Perforation Test: Negative at 28 days.<br />
Key Features: culture characteristics, microscopic morphology and failure to perforate<br />
hair “in vitro”.<br />
20 µm<br />
Typical slender clavate microconidia of Trichophyton rubrum downy type.
160<br />
Descriptions of Medical Fungi<br />
Colonies (SDA) are flat to slightly raised, white to cream, suede-like with a pinkish-red<br />
reverse. Microscopically, most cultures have numerous clavate to pyriform microconidia<br />
and moderate numbers of smooth, thin-walled multiseptate, slender cylindrical<br />
macroconidia. Older cultures may show numerous chlamydospores with few clavate<br />
to pyriform microconidia.<br />
Kaminski’s Dermatophyte Identification Scheme<br />
Littman Oxgall Agar: Raised, greyish, suede-like colonies with some radial folding<br />
and a greenish-yellow diffusible pigment.<br />
Lactritmel Agar: Flat, white to rose pink, suede-like to granular colonies with a pinkish<br />
to wine-red reverse. Numerous broad clavate to pyriform microconidia and moderate<br />
numbers of smooth, thin-walled, slender cylindrical macroconidia are present. A few<br />
chlamydospores may be present in older cultures.<br />
Sabouraud’s Dextrose Agar with 5% NaCl: A very stunted, heaped and folded,<br />
glabrous, cream thallus, later developing a dark red central spot. Reverse is a brownishyellow<br />
colour.<br />
1% Peptone Agar: Flat, white to cream, glabrous to suede-like colony with no reverse<br />
pigment.<br />
Hydrolysis of Urea: Positive at 7 days<br />
Vitamin Free Agar (Trichophyton Agar No.1): Good growth indicating no special<br />
nutritional requirements. White to cream suede-like colonies with a pinkish-red to<br />
wine-red reverse.<br />
Hair Perforation Test: Positive.<br />
Trichophyton rubrum granular type<br />
Key Features: culture characteristics and microscopic morphology.<br />
Culture of Trichophyton rubrum granular strain.
Descriptions of Medical Fungi 161<br />
20 µm<br />
Trichophyton rubrum granular type<br />
20 µm<br />
Macroconidia and microconidia of Trichophyton rubrum granular type.
162<br />
Descriptions of Medical Fungi<br />
Trichophyton schoenleinii (Lebert) Langeron & Milochevitch<br />
Colonies (SDA) are slow growing, waxy or suede-like with a deeply folded honeycomb-like<br />
thallus and some sub-surface growth. The thallus is cream-coloured to yellow<br />
to orange brown. Cultures are difficult to maintain in their typical convoluted form,<br />
and rapidly become flat and downy. No reverse pigmentation is present. No macroconidia<br />
and microconidia are seen in routine cultures, however numerous chlamydospores<br />
may be present in older cultures. However, characteristic antler “nail head”<br />
hyphae also known as “favic chandeliers” may be observed. A few distorted clavate<br />
microconidia may be formed by some isolates when grown on polished rice grains.<br />
RG-2 organism<br />
Key Features: clinical history, culture characteristics and microscopic morphology<br />
showing favic chandeliers.<br />
20 µm<br />
Culture and “favic chandeliers” of Trichophyton schoenleinii.<br />
Trichophyton schoenleinii is an anthropophilic fungus causing favus in humans. Favus<br />
is a chronic, scarring form of tinea capitis characterised by saucer-shaped crusted lesions<br />
or scutula and permanent hair loss. Invaded hairs remain intact and fluoresce<br />
a pale greenish yellow under Wood’s ultra-violet light. Favus was once common in<br />
Eurasia and North Africa, however its incidence is now in decline.
Descriptions of Medical Fungi 163<br />
Trichophyton soudanense Joyeux.<br />
Colonies (SDA) are slow-growing with a flat to folded, suede-like surface. Often there<br />
is a broad fringe of submerged growth. The surface mycelium and reverse pigment are<br />
characteristically a deep apricot-orange in colour. Microscopically, the hyphae often<br />
show reflexive or right-angle branching. Pyriform microconidia may occasionally be<br />
present and numerous chlamydospores are often found in older cultures. On BCPmilk<br />
solids agar, a thin halo of clearing usually appears in the milk solids around the<br />
colony edge at 7-10 days. RG-2 organism.<br />
T. soudanense appears to be genetically related to Trichophyton rubrum and T. violaceum<br />
(Graser et al. 2007), however we have maintained the current description until<br />
the taxonomy is clarified.<br />
Key Features: clinical history, culture characteristics and microscopic morphology<br />
showing reflexive hyphal branching and endothrix invasion of hair.<br />
20 µm<br />
Culture and “reflexive” hyphal branching in Trichophyton soudanense.<br />
Trichophyton soudanense is an anthropophilic fungus which is a frequent cause of<br />
tinea capitis in Africa. Invaded hairs show an endothrix infection but do not fluoresce<br />
under Wood’s ultra-violet light. Distribution is mainly in Africa with imported cases now<br />
reported from Europe, Brazil, Australia and USA.
164<br />
Descriptions of Medical Fungi<br />
Trichophyton terrestre Durie and Frey<br />
Teleomorphs: Arthroderma insingulare Padhye and Carmichael<br />
Arthroderma lenticulare Pore, Tsao and Plunkett<br />
Arthroderma quadrifidum Dawson and Gentles<br />
Colonies (SDA) are usually flat to downy with a suede-like to granular texture resembling<br />
T. mentagrophytes. The surface colour may range from white to cream, buff to<br />
yellow, or greenish-yellow. Reverse pigmentation is usually yellowish-brown although<br />
some variants have a deep rose-red reverse. Microconidia are large, clavate or pedicellate,<br />
usually exhibiting transition forms to more or less abundant lateral macroconidia.<br />
Macroconidia are clavate to cylindrical with rounded ends, smooth and thin-walled,<br />
and are two- to six-celled. Chlamydospores, hyphal spirals, racquet mycelium and<br />
antler hyphae may also be present. No growth at 37 O C. RG-1 organism.<br />
Trichophyton terrestre is a geophilic fungus of world-wide distribution which may occur<br />
as a saprophytic contaminant on humans and animals. It is not known to invade hair<br />
in vivo, but produces hair perforations in vitro.<br />
Key Features: culture characteristics and microscopic morphology.<br />
20 µm<br />
Culture and macroconidia of Trichophyton terrestre.
Descriptions of Medical Fungi 165<br />
Colonies (SDA) show considerable variation in texture and colour. They may be suedelike<br />
to powdery, flat with a raised centre or folded, often with radial grooves. The colour<br />
may vary from pale-buff to yellow, (the sulfureum form which resembles Epidermophyton<br />
floccosum), to dark-brown. The reverse colour varies from yellow-brown to reddish-brown<br />
to deep mahogany. Hyphae are relatively broad, irregular, much branched<br />
with numerous septa. Numerous characteristic microconidia varying in size and shape<br />
from long clavate to broad pyriform, are borne at right angles to the hyphae, which often<br />
remain unstained by lactophenol cotton blue. Very occasional smooth, thin-walled,<br />
irregular, clavate macroconidia may be present on some cultures. Numerous swollen<br />
giant forms of microconidia and chlamydospores are produced in older cultures. RG-2<br />
organism.<br />
Kaminski’s Dermatophyte Identification Scheme<br />
Littman Oxgall Agar: Restricted colony with cream, sometimes greyish, suede-like<br />
folded surface with no reverse pigment.<br />
Lactritmel Agar: Macroscopic and microscopic features as described above for the<br />
primary culture.<br />
Sabouraud’s Dextrose Agar with 5% NaCl: Very stunted slow growing colony with<br />
dark brown surface and reverse.<br />
1% Peptone Agar: Flat, white to cream suede-like surface with raised centre. No<br />
reverse pigment.<br />
Hydrolysis of Urea: positive at 5 days<br />
Trichophyton tonsurans Malmsten<br />
Nutritional Tests on Trichophyton Agars: results demonstrate a partial requirement<br />
for thiamine. T1 = vitamin free agar, T4 = vitamin free + thiamine agar.<br />
Hair Perforation Test: Positive within 14 days.<br />
T1 T4<br />
Key Features: microscopic morphology, culture characteristics, endothrix invasion of<br />
hairs and partial thiamine requirement.<br />
Trichophyton tonsurans is an anthropophilic fungus with a world wide distribution which<br />
causes inflammatory or chronic non-inflammatory finely scaling lesions of skin, nails<br />
and scalp. It is a common cause of tinea capitis in the Australian Aborigine and African<br />
Americans. Invaded hairs show an endothrix infection and do not fluoresce under<br />
Wood’s ultra-violet light.
166<br />
Descriptions of Medical Fungi<br />
Trichophyton tonsurans Malmsten<br />
20 µm<br />
Colonies, hyphae, microconidia and macroconidia of Trichophyton tonsurans.
Descriptions of Medical Fungi 167<br />
Teleomorph: Arthroderma benhamiae Ajello & Chang.<br />
Colonies (SDA) are slow growing, small, button or disc-shaped, white to cream-coloured,<br />
with a suede-like to velvety surface, a raised centre, and flat periphery with<br />
some submerged growth. Reverse pigment may vary from non-pigmented to yellow.<br />
Broad, irregular hyphae with many terminal and intercalary chlamydospores are<br />
present. Chlamydospores are often in chains. The tips of some hyphae are broad<br />
and club-shaped, and occasionally divided, giving the so-called “antler” effect. When<br />
grown on thiamine-enriched media, occasional strains produce clavate to pyriform microconidia<br />
borne singly along the hyphae. Macroconidia are only rarely produced, but<br />
when present have a characteristic tail or string-bean shape. RG-2 organism.<br />
Confirmatory Tests:<br />
Trichophyton verrucosum Bodin<br />
Growth at 37 O C: unlike other dermatophytes growth is enhanced at 37 O C<br />
Nutritional Requirements: all strains require thiamine and approximately 80% require<br />
thiamine and inositol. There is no growth on casein vitamin free agar (T1), minimal<br />
submerged growth on T1 + inositol (T2), good growth on T1 + inositol and thiamine<br />
(T3) and good growth on T1 + thiamine only (T4).<br />
All strains produce typical chains of chlamydospores, often referred to as “chains of<br />
pearls”, especially when grown on BCP milk solids glucose agar at 37 O C. Also when<br />
grown at 25 O C on milk solids glucose agar a halo of peripheral clearing of milk solids<br />
occurs within 7 days.<br />
Microscopic examination of young 4 to 5 day old colonies, grown from a very small<br />
inoculum, on Sabouraud’s’ dextrose agar containing 0.5% yeast extract and incubated<br />
at 30 O C, show characteristic terminal vesicles (not chlamydospores) at the tips of<br />
hyphae. The number of vesicles produced is greater from primary inoculations of skin<br />
scrapings or hairs.<br />
Key Features: culture characteristics and requirements for thiamine and inositol, large<br />
ectothrix invasion of hair, clinical lesions and history.<br />
Trichophyton verrucosum is a zoophilic fungus causing ringworm in cattle. Infections<br />
in humans result from direct contact with cattle or infected fomites and are usually<br />
highly inflammatory involving the scalp, beard or exposed areas of the body (ie. nails,<br />
skin). Invaded hairs show an ectothrix infection and fluorescence under Wood’s ultraviolet<br />
light has been noted in cattle but not in humans. Geographic distribution is<br />
world-wide.
168<br />
Descriptions of Medical Fungi<br />
Trichophyton verrucosum Bodin<br />
20 µm<br />
20 µm<br />
30 µm<br />
20 µm<br />
Trichophyton verrucosum showing clavate to pyriform microconidia,<br />
characteristic rat tail or string bean-shaped macroconidia, terminal vesicles<br />
at the tips of hyphae in young colonies and chains of chlamydospores.
Descriptions of Medical Fungi 169<br />
Trichophyton violaceum Sabouraud apud Bodin<br />
Colonies (SDA) are very slow growing, glabrous or waxy, heaped and folded and a<br />
deep violet in colour. Cultures often become pleomorphic, forming white sectors and<br />
occasional non-pigmented strains may occur. Hyphae are relatively broad, tortuous,<br />
much branched and distorted. Young hyphae usually stain well in lactophenol cotton<br />
blue, whereas older hyphae stain poorly and show small central fat globules and granules.<br />
No conidia are usually seen, although occasional pyriform microconidia have<br />
been observed on enriched media. Numerous chlamydospores are usually present,<br />
especially in older cultures. RG-2 organism.<br />
Nutritional Requirements: T. violaceum has a partial nutrient requirement for thiamine.<br />
There is minimal growth on casein vitamin-free agar (Trichophyton Agar No. 1),<br />
and slightly better growth on vitamin-free agar plus thiamine (Trichophyton Agar No.<br />
4). The partial requirement for thiamine separates this organism from T. gourvillii, T.<br />
rubrum, and other species that may produce purple pigmented colonies.<br />
Key Features: culture characteristics, partial thiamine requirement and endothrix hair<br />
invasion.<br />
Culture and chlamydospores of Trichophyton violaceum.<br />
20 µm<br />
Trichophyton violaceum is an anthropophilic fungus causing inflammatory or chronic<br />
non-inflammatory finely scaling lesions of skin, nails, beard and scalp, producing the<br />
so-called “black dot” tinea capitis. Distribution is world-wide, particularly in the Near<br />
East, Eastern Europe, USSR and North Africa. Invaded hairs show an endothrix<br />
infection and do not fluoresce under Wood’s ultra-violet light.
170<br />
Descriptions of Medical Fungi<br />
Trichosporon Behrend<br />
The genus Trichosporon is characterised by the development of hyaline, septate hyphae<br />
that fragment into oval or rectangular arthroconidia. Some blastoconidia are also<br />
seen. The colonies are usually raised and have a waxy appearance, which develop<br />
radial furrows and irregular folds.<br />
Following recent molecular studies, the genus has undergone major revision (Gueho<br />
et al. 1992, de Hoog et al. 2000, Rodriguez-Tudela et al. 2005) and 6 species of medical<br />
importance are described below. In particular, the name Trichosporon beigelii is<br />
now obsolete, and previously described infections reported in the literature under this<br />
name could in fact be due to any one of the species listed below.<br />
Trichosporon species are a minor component of normal skin flora, and are widely distributed<br />
in nature. They are regularly associated with the soft nodules of white piedra,<br />
and have been involved in a variety of opportunistic infections in the immunosuppressed<br />
patient. Disseminated infections are most frequently caused by T. asahii<br />
and have been associated with leukaemia, organ transplantation, multiple myeloma,<br />
aplastic anaemia, lymphoma, solid tumours and AIDS. Disseminated infections are<br />
often fulminate and widespread, with lesions occurring in the liver, spleen, lungs and<br />
gastrointestinal tract. Infections in non-immunosuppressed patients include endophthalmitis<br />
after surgical extraction of cataracts, endocarditis usually following insertion<br />
of prosthetic cardiac valves, peritonitis in patients on continuous ambulatory peritoneal<br />
dialysis (CAPD), and intravenous drug abuse.<br />
For descriptions of species, keys to taxa and additional information see Kurtzman<br />
and Fell (1988), Gueho et al. (1992), de Hoog et al. (2000), Rodriguez-Tudela et al.<br />
(2005).<br />
Key to medically important species (de Hoog et al. 2000).<br />
1. Growth with melibiose 2<br />
No growth with melibiose 3<br />
2. Tolerant to cycloheximide T. mucoides<br />
Not tolerant to cycloheximide T. cutaneum<br />
3. Growth with myo-inositol, no growth with L-arabinose T. inkin<br />
No growth with myo-inositol, growth with L-arabinose 4<br />
4. Colony with very slow growth; thallus consisting of clumps<br />
of meristematic cells (sarcinae) T. asteroides<br />
Colonies and microscopy otherwise 5<br />
5. Appressoria present in slide cultures T. ovoides<br />
Appressoria absent in slide cultures 6<br />
6. Arthroconidia barrel-shaped; thallus not meristematic T. asahii<br />
Arthroconidia elongate, or thallus meristematic T. asteroides
Descriptions of Medical Fungi 171<br />
Trichosporon asahii Akagi ex Sugita et al.<br />
Colonies (SDA) are white to cream-coloured, powdery, suede-like to farinose with radial<br />
furrows and irregular folds. Budding cells and lateral conidia are absent. Arthroconidia<br />
are barrel-shaped. Appressoria absent. This species assimilates L-arabinose<br />
but not melibiose. Growth at 37 O C. Most common species, especially from invasive<br />
infections. RG-2 organism.<br />
Assimilation Tests: + Positive, - Negative, v Variable, w Weak, s Slow<br />
Glucose + Melibiose - L-Rhamnose + D-Glucitol v<br />
Galactose + Raffinose - D-Glucosamine + α-M-D-glucoside +<br />
L-Sorbose v Melezitose v N-A-D-glucosamine + D-Gluconate +<br />
Sucrose v Soluble Starch v Glycerol v DL-Lactate v<br />
Maltose + D-Xylose v Erythritol + myo-Inositol v<br />
Cellobiose + L-Arabinose + Ribitol v Nitrate -<br />
Trehalose + D-Arabinose + Galactitol - 2-K-D-gluconate +<br />
Lactose + D-Ribose + D-Mannitol v D-Glucuronate +<br />
Culture, hyphae and arthroconidia of Trichosporon asahii.<br />
20 µm<br />
Antifungal<br />
MIC µg/mL<br />
Range MIC90 Antifungal<br />
MIC µg/mL<br />
Range MIC90 Fluconazole 0.25-16 8.0 Amphotericin B 0.25-16 8.0<br />
Itraconazole 0.03-16 0.5 Flucytosine 2-128 16<br />
Posaconazole 0.06-16 1.0 Caspofungin >8 >8<br />
Voriconazole 0.03-16 0.25 Anidulafungin >8 >8<br />
MIC data for T. asahii. Antifungal susceptibility may vary between species and<br />
resistant strains have been reported. Therefore, antifungal susceptibility testing of<br />
individual strains is recommended. Paphitou et al. (2002), Espinel-Ingroff (2003),<br />
Rodriguez-Tudela et al. (2005), Metin et al. (2005) and WCH in-house data.
172<br />
Descriptions of Medical Fungi<br />
Trichosporon asteroides (Rischin) Ota<br />
Colonies (SDA) are restricted, dry, cream-coloured, cerebriform, with radial furrows<br />
and irregular folds. The meristematic form is punctiform, brownish and consists of hyphae<br />
which swell and become multiseptate which may fall apart into smaller packets.<br />
Budding cells and lateral conidia are absent. Arthroconidia are elongate and hyphae<br />
are often present. Appressoria absent. This species assimilates L-arabinose but not<br />
myo-inositol. Growth at 37 O C is variable. Uncommon species usually associated with<br />
superficial infections. RG-2 organism.<br />
Assimilation Tests: + Positive, - Negative, v Variable, w Weak, s Slow<br />
Glucose + Melibiose - L-Rhamnose + D-Glucitol v<br />
Galactose + Raffinose - D-Glucosamine v α-M-D-glucoside +<br />
L-Sorbose v Melezitose + N-A-D-glucosamine + D-Gluconate +<br />
Sucrose + Soluble Starch + Glycerol + DL-Lactate +<br />
Maltose + D-Xylose + Erythritol + myo-Inositol -<br />
Cellobiose + L-Arabinose + Ribitol v Nitrate -<br />
Trehalose + D-Arabinose + Galactitol - 2-K-D-gluconate +<br />
Lactose + D-Ribose + D-Mannitol v D-Glucuronate +<br />
Trichosporon cutaneum (de Beurmann et al.) Ota<br />
Colonies (SDA) are cream-coloured, cerebriform, glabrous, with radial furrows and irregular<br />
folds. Budding cells abundant in primary cultures; hyphae developing in older<br />
cultures. Arthroconidia are cylindrical to ellipsoidal. Appressoria absent. This species<br />
assimilates melibiose; not tolerant to 0.1% cycloheximide. No growth at 37 O C. Uncommon<br />
species usually associated with superficial infections. RG-2 organism.<br />
Assimilation Tests: + Positive, - Negative, v Variable, w Weak, s Slow<br />
Glucose + Melibiose + L-Rhamnose + D-Glucitol +<br />
Galactose + Raffinose + D-Glucosamine v α-M-D-glucoside +<br />
L-Sorbose v Melezitose + N-A-D-glucosamine + D-Gluconate +<br />
Sucrose + Soluble Starch + Glycerol + DL-Lactate +<br />
Maltose + D-Xylose + Erythritol + myo-Inositol +<br />
Cellobiose + L-Arabinose + Ribitol + Nitrate -<br />
Trehalose + D-Arabinose v Galactitol - 2-K-D-gluconate +<br />
Lactose + D-Ribose + D-Mannitol + D-Glucuronate +<br />
Trichosporon inkin (Oho ex Ota) do Carmo-Sousa & van Uden<br />
Colonies (SDA) are restricted, white, finely cerebriform with a granular covering, without<br />
marginal zone, often cracking the media. Budding cells and lateral conidia absent.<br />
Arthroconidia are long cylindrical. Appressoria present in slide cultures. Sarcinae<br />
present on media with high sugar-content. This species assimilates myo-inositol but<br />
not melibiose. Growth at 37 O C. Usually associated with white piedra on pubic hairs.<br />
RG-2 organism.
Descriptions of Medical Fungi 173<br />
Trichosporon inkin (Oho ex Ota) do Carmo-Sousa & van Uden<br />
Assimilation Tests: + Positive, - Negative, v Variable, w Weak, s Slow<br />
Glucose + Melibiose - L-Rhamnose - D-Glucitol -<br />
Galactose v Raffinose - D-Glucosamine v α-M-D-glucoside +<br />
L-Sorbose v Melezitose + N-A-D-glucosamine + D-Gluconate +<br />
Sucrose + Soluble Starch + Glycerol v DL-Lactate +<br />
Maltose + D-Xylose + Erythritol + myo-Inositol +<br />
Cellobiose + L-Arabinose v Ribitol - Nitrate -<br />
Trehalose + D-Arabinose v Galactitol - 2-K-D-gluconate +<br />
Lactose + D-Ribose + D-Mannitol v D-Glucuronate +<br />
Trichosporon mucoides Gueho & M.Th. Smith<br />
Colonies (SDA) are moist and glabrous, white, cerebriform, heaped and folded. Budding<br />
cells present in primary cultures. Broadly clavate, terminal or lateral blastoconidia<br />
often present, becoming thick-walled with age. Arthroconidia are barrel-shaped. Appressoria<br />
absent. This species assimilates melibiose and is tolerant to 0.1% cycloheximide.<br />
Growth at 37 O C. Common species associated with superficial infections, white<br />
piedra and onychomycosis. RG-2 organism.<br />
Assimilation Tests: + Positive, - Negative, v Variable, w Weak, s Slow<br />
Glucose + Melibiose + L-Rhamnose + D-Glucitol +<br />
Galactose + Raffinose + D-Glucosamine + α-M-D-glucoside +<br />
L-Sorbose + Melezitose + N-A-D-glucosamine + D-Gluconate +<br />
Sucrose + Soluble Starch + Glycerol + DL-Lactate +<br />
Maltose + D-Xylose + Erythritol + myo-Inositol +<br />
Cellobiose + L-Arabinose + Ribitol + Nitrate -<br />
Trehalose + D-Arabinose + Galactitol + 2-K-D-gluconate +<br />
Lactose + D-Ribose + D-Mannitol + D-Glucuronate +<br />
Trichosporon ovoides Behrend<br />
Colonies (SDA) are restricted, white, granular, folded at the centre, with a flat marginal<br />
zone. Budding cells and lateral conidia absent. Arthroconidia are cylindrical. Appressoria<br />
present in slide cultures. This species does not assimilate melibiose, but tolerates<br />
0.1% cycloheximide. Growth at 37 O C is variable. Uncommon species usually<br />
associated with superficial infections, like white piedra. RG-2 organism.<br />
Assimilation Tests: + Positive, - Negative, v Variable, w Weak, s Slow<br />
Glucose + Melibiose - L-Rhamnose + D-Glucitol v<br />
Galactose + Raffinose v D-Glucosamine v α-M-D-glucoside +<br />
L-Sorbose v Melezitose v N-A-D-glucosamine + D-Gluconate +<br />
Sucrose + Soluble Starch + Glycerol v DL-Lactate +<br />
Maltose + D-Xylose + Erythritol + myo-Inositol +<br />
Cellobiose + L-Arabinose v Ribitol - Nitrate -<br />
Trehalose v D-Arabinose v Galactitol - 2-K-D-gluconate +<br />
Lactose + D-Ribose + D-Mannitol + D-Glucuronate +
174<br />
Descriptions of Medical Fungi<br />
Trichothecium roseum (Persoon) Link ex Gray<br />
Colonies are moderately fast growing, flat, suede-like to powdery, initially white but<br />
becoming rosy, pink or orange with age. The conidiophores are indistinguishable<br />
from the vegetative hyphae until the first conidium is produced. They are erect, unbranched,<br />
often septate near the base, more or less rough-walled, bearing basipetal<br />
zig-zag (alternating) chains of conidia at the apex. Note: the conidiophore is progressively<br />
shortened with the formation of each conidium i.e. retrogressive conidial development.<br />
Conidia are two-celled ellipsoidal to pyriform, with an obliquely truncate basal<br />
scar, hyaline, smooth to delicately roughened and thick-walled.<br />
Trichothecium roseum has a world-wide distribution and is often isolated from decaying<br />
plant substrates, soil, seeds of corn, and food-stuffs (especially flour products). It<br />
is occasionally isolated as a saprophyte in the clinical laboratory. RG-1 organism.<br />
Trichothecium roseum should not be confused with Microsporum nanum. Colonies of<br />
the latter may be pinkish-buff in colour and also produce ovoid to pear-shaped, mostly<br />
two-celled macroconidia with thin, verrucose walls. However, M. nanum usually produces<br />
a red-brown reverse pigment and the two-celled macroconidia are sessile and<br />
formed singly, sometimes on stalks, on undifferentiated conidiophores which do not<br />
undergo further change or produce secondary conidia. Note: conidia are not produced<br />
in basipetal chains as in T. roseum. Finally, M. nanum will perforate hair in vitro.<br />
Key Features: hyphomycete, basipetal zig-zag chains of two-celled conidia showing<br />
retrogressive development where the conidiophore becomes progressively shorter.<br />
For descriptions of species, keys to taxa and additional information see McGinnis<br />
(1980), Domsch et al. (1980), Rippon (1988) and Samson et al. (1995).<br />
20 µm<br />
Conidiophores of T. roseum demonstrating retrogressive conidial development.
Descriptions of Medical Fungi 175<br />
Ulocladium Preuss<br />
Colonies are rapid growing, brown to olivaceous-black or greyish and suede-like to<br />
floccose. Microscopically, numerous, usually solitary, multi-celled conidia (dictyoconidia)<br />
are formed through a pore (poroconidia) by a sympodially elongating geniculate<br />
conidiophore. Conidia are typically obovoid (narrowest at the base), dark brown and<br />
often rough-walled. Seven species have been described, all being saprophytes. RG-<br />
1 organism.<br />
Species of Ulocladium should not be confused with other poroconidial genera such as<br />
Stemphylium, Alternaria, Bipolaris, Exserohilum, Dreschlera and Curvularia.<br />
For descriptions of species, keys to taxa and additional information see Ellis (1970 and<br />
1976), Domsch et al. (1980), Rippon (1988), Samson et al. (1995) and de Hoog et al.<br />
(2000).<br />
Antifungal<br />
Conidia of Ulocladium.<br />
10 µm<br />
MIC µg/mL<br />
MIC µg/mL<br />
Antifungal<br />
Range Range<br />
Fluconazole 8->64 Amphotericin B 1->16<br />
Itraconazole 0.06->16 Flucytosine >128<br />
Voriconazole 0.25<br />
Very limited data. Antifungal susceptibility testing of individual strains is<br />
recommended. Pujol et al. (2000) and WCH in-house data.
176<br />
Descriptions of Medical Fungi<br />
Veronaea botryosa Ciferri & Montemartini<br />
Colonies grow rapidly and are suede-like to downy, greyish-brown to blackish-brown.<br />
Conidiophores are erect, straight or flexuose, occasionally branched and are usually<br />
geniculate, due to the sympodial development of the conidia. They are smooth-walled,<br />
pale to medium olivaceous-brown, up to 250 µm long and 2-4 µm wide. Conidia are<br />
pale brown, two-celled, cylindrical with a truncated base, smooth-walled or slightly verrucose,<br />
5-12 x 3-4 µm. RG-1 organism.<br />
This genus is very similar to Rhinocladiella, however the conidia are typically twocelled.<br />
Occasional skin infections have been reported from humans.<br />
For descriptions of species, keys to taxa and additional information see Ellis (1971)<br />
and de Hoog et al. (2000).<br />
Conidiophores and conidia of Veronaea botryosa.<br />
10 µm
Descriptions of Medical Fungi 177<br />
Verticillium Nees ex Link<br />
Colonies are fast growing, suede-like to downy, white to pale yellow in colour, becoming<br />
pinkish brown, red, green or yellow with a colourless, yellow or reddish brown reverse.<br />
Conidiophores are usually well differentiated and erect, verticillately branched<br />
over most of their length, bearing whorls of slender awl-shaped divergent phialides.<br />
Conidia are hyaline or brightly coloured, mostly one-celled, and are usually borne in<br />
slimy heads (glioconidia).<br />
Members of this genus are often isolated from the environment. It has been reported<br />
as a rare agent of mycotic keratitis. RG-1 organism.<br />
Key Features: hyphomycete, verticillate branched conidiophores bearing whorls of<br />
awl-shaped, divergent phialides.<br />
For descriptions of species, keys to taxa and additional information see Domsch et al.<br />
(1980), McGinnis (1980), Rippon (1988), Samson et al. (1995), de Hoog et al. (2000).<br />
20 µm<br />
Conidiophores, phialides and conidia of Verticillium.
178<br />
Descriptions of Medical Fungi<br />
Calcofluor White with 10% KOH.<br />
For the direct microscopic examination of skin scrapings, hairs, nails and other clinical<br />
specimens for fungal elements. This as a very sensitive method, however, a fluorescence<br />
microscope with the correct ultraviolet filters is required (Hageage and Harrington,<br />
1984; Hollander et al., 1984; Monheit et al., 1984).<br />
Solution A: Potassium hydroxide reagent.<br />
Potassium hydroxide 10 g<br />
Glycerine 10 mL<br />
Distilled water 80 mL<br />
Solution B: Calcofluor white reagent.<br />
Calcofluor white 0.5 g<br />
Evans blue 0.02 g<br />
Distilled water 50 mL<br />
Mix one drop of each solution on the centre of a clean microscope slide.<br />
Place the specimen in the solution and cover with a coverslip.<br />
Potassium Hydroxide (KOH) with Chlorazol Black.<br />
For the direct microscopic examination of skin scrapings, hairs, nails and other clinical<br />
specimens for fungal elements. Note: Parker Quink ink is no longer available.<br />
Potassium hydroxide 10 g<br />
Coral Azole E Black (0.1% - 100mg in 100ml) 10 mL<br />
Glycerol 10 mL<br />
Distilled water 80 mL<br />
Using sterile technique, remove a small portion of the specimen with an<br />
inoculation needle and mount in a drop of KOH on a clean microscope<br />
slide. Cover with a coverslip, squash the preparation with the butt of the<br />
inoculation needle and then blot off the excess fluid.<br />
Indian Ink Mounts.<br />
MICROSCOPY STAINS & TECHNIQUES<br />
For the direct microscopic examination of CSF for Cryptococcus species. Place a drop<br />
of Indian Ink on the specimen, mix well with a sterilised loop, and cover with a coverslip.<br />
Best brands to use are “Pelikan” or “Talons” Indian Ink.
Descriptions of Medical Fungi 179<br />
Lactophenol Cotton Blue (LPCB).<br />
For the staining and microscopic identification of fungi.<br />
Cotton Blue (Aniline Blue) 0.05 g<br />
Phenol Crystals (C 6 H 5 O 4 ) 20 g<br />
Glycerol 40 mL<br />
Lactic acid (CH 3 CHOH COOH) 20 mL<br />
Distilled water 20 mL<br />
This stain is prepared over two days.<br />
1. On the first day, dissolve the Cotton Blue in the distilled water. Leave<br />
overnight to eliminate insoluble dye.<br />
2. On the second day, wearing gloves add the phenol crystals to the lactic<br />
acid in a glass beaker. Place on magnetic stirrer until the phenol is<br />
dissolved.<br />
3. Add the glycerol.<br />
4. Filter the Cotton Blue and distilled water solution into the phenol/glycerol/<br />
lactic acid solution. Mix and store at room temperature.<br />
Direct Microscopic Mounts or Squash Preparations.<br />
Using sterile technique, remove a small portion of the colony with an inoculation needle<br />
and mount in a drop of Lactophenol Cotton Blue on a clean microscope slide.<br />
Cover with a coverslip, squash the preparation with the butt of the inoculation needle<br />
and then blot off the excess fluid.<br />
Cellotape Flag Preparations.<br />
MICROSCOPY STAINS & TECHNIQUES<br />
An excellent technique for the rapid mounting of sporulating fungi because it keeps<br />
more of the reproductive structures intact.<br />
1. Using clear 2cm wide cellotape and a wooden applicator stick (orange<br />
stick) make a small cellotape flag (2 x 2 cm).<br />
2. Using sterile technique, gently press the sticky side of the flag onto the<br />
surface of the culture.<br />
3. Remove and apply a drop of 95% alcohol to the flag, this acts as a wetting<br />
agent and also dissolves the adhesive glue holding the flag to the<br />
applicator stick.<br />
4. Place the flag onto a small drop of Lactophenol cotton blue on a clean<br />
glass slide, remove the applicator stick and discard, add another drop<br />
of stain, cover with a coverslip, gently press and mop up any excess<br />
stain.
180<br />
Descriptions of Medical Fungi<br />
Slide Culture Preparations.<br />
MICROSCOPY STAINS & TECHNIQUES<br />
In order to accurately identify many fungi it is essential to observe the precise arrangement<br />
of the conidiophores and the way in which spores are produced (conidial ontogeny).<br />
Riddel’s simple method of slide culturing (Mycologia 42:265, 1950) permits fungi<br />
to be studied virtually in situ with as little disturbance as possible. A simple modification<br />
of this method using a single agar plate is described below.<br />
One plate of nutrient agar; potato dextrose is recommended, however,<br />
some fastidious fungi may require harsher media to induce sporulation like<br />
Cornmeal agar or Czapek Dox agar.<br />
1. Using a sterile blade cut out an agar block (7 x 7 mm) small enough to<br />
fit under a coverslip.<br />
2. Flip the block up onto the surface of the agar plate.<br />
3. Inoculate the four sides of the agar block with spores or mycelial<br />
fragments of the fungus to be grown.<br />
4. Place a flamed coverslip centrally upon the agar block.<br />
5. Incubate the plate at 26 O C until growth and sporulation have<br />
occurred.<br />
6. Remove the cover slip from the agar block.<br />
7. Apply a drop of 95% alcohol as a wetting agent.<br />
8. Gently lower the coverslip onto a small drop of Lactophenol cotton blue<br />
on a clean glass slide.<br />
9. The slide can be left overnight to dry and later sealed with fingernail<br />
polish.<br />
10. When sealing with nail polish use a coat of clear polish followed by one<br />
coat of red-coloured polish.<br />
Simple agar block method, inoculated on four sides with cover slip<br />
on top. Make at least 2 slides per culture.
Descriptions of Medical Fungi 181<br />
Bird Seed Agar (Staib, 1987).<br />
for selective isolation of Cryptococcus neoformans and C. gattii.<br />
Guizotia abyssinica (niger seed) 50 g Glucose 1 g<br />
KH PO (potassium dihydrogen 1 g Creatinine 1 g<br />
2 4<br />
orthophosphate)<br />
Bacto Agar (BD 214010) 15 g Distilled water 1000 mL<br />
Penicillin G (20 units/mL) 1 mL Gentamicin (40 mg/mL) 1 mL<br />
1. Grind seeds of Guizotia abyssinica as finely as possible with an electric mixer<br />
and add to 1000 mL distilled water in a stainless steel jug.<br />
2. Boil for 30 minutes, pass through filter paper and adjust volume to 1000 mL.<br />
3. Add remaining ingredients except Bacto Agar to filtrate and dissolve.<br />
If required: Cool to room temperature and adjust pH to 5.5.<br />
Dispense into 500 mL bottles.<br />
4. Add 7.5 g Bacto Agar to each 500 mL reagent bottle.<br />
5. Autoclave 110OC for 20 minutes.<br />
6. Cool to 48OC and add 0.5 mL Penicillin G and 0.5 mL Gentamicin to each 500<br />
mL of Bird Seed Agar.<br />
7. Mix gently and pour into 90 mm plastic petri dishes.<br />
Bromcresol Purple Milk Solids Glucose Agar (BCP-MS-G).<br />
for the differentiation of Trichophyton species (Kane et al. 1977).<br />
Solution A:<br />
Distilled water 1000 mL<br />
Skim milk powder (Carnation Brand) 80 g<br />
Bromcresol (or bromocresol) purple<br />
2 mL<br />
(1.6% solution in alcohol)<br />
Dissolve in 2 litre flask and autoclave 10 psi/15 minutes.<br />
Solution B:<br />
Glucose 40 g Distilled water 200 mL<br />
Dissolve and autoclave at 10 psi/8minutes.<br />
Solution C:<br />
SPECIALISED CULTURE MEDIA<br />
Bacto Agar (BD 214010) 30 g Distilled water 800 mL<br />
Soak for 15 minutes in 3 litre flask; autoclave at 15 psi/15 minutes<br />
To make media; add solution A and B to solution C. Adjust final pH to 6.6.<br />
Aseptically dispense for slopes (7 mL amounts into 30 mL disposable bottles).<br />
Caution: Do not substitute casein for skim milk. Check pH is 6.6.
182<br />
Descriptions of Medical Fungi<br />
CDBT (Creatinine dextrose bromothymol blue thymine agar).<br />
for differentiation of Cryptococcus neoformans var. neoformans and<br />
Cryptococcus neoformans var. grubii (Irokanulo et al. 1994).<br />
Solution A:<br />
Creatinine 1 g Dextrose 0.5 g<br />
KH 2 PO 4 1 g MgSO 4 7H 2 O 0.5 g<br />
Thymine 0.1 g Distilled water 980 mL<br />
1. Dissolve ingredients in small beaker and adjust pH to 5.6<br />
2. Store in refrigerator.<br />
Solution B (Aqueous Bromothymol Blue):<br />
Bromothymol blue 0.4 g 0.01N NaOH 64 mL<br />
Distilled water 36 mL<br />
1. Dissolve the Bromothymol Blue in the NaOH<br />
2. Add to the water.<br />
To prepare medium (1 litre for plates):<br />
Solution A 980 mL Solution B 20 mL<br />
Bacto Agar (BD 214010) 20 g<br />
Autoclave to 121 O C for 15 minutes, cool to 48 O C and pour plates.<br />
CGB (L-Canavanine glycine bromothymol blue agar).<br />
for differentiation of Cryptococcus neoformans and Cryptococcus gattii<br />
(Kwon-Chung et al. 1982).<br />
Solution A:<br />
Glycine Univar 10 g KH 2 PO 4 1 g<br />
MgSO 4 1 g Thiamine HCl 1 mg<br />
L-canavanine sulphate 30 mg Distilled water 100 mL<br />
1. Dissolve ingredients in small beaker and adjust pH to 5.6<br />
2. Filter sterilise solution using 0.22 µm filter.<br />
3. Store in refrigerator.<br />
Solution B (Aqueous Bromothymol Blue):<br />
Bromothymol blue 0.4 g 0.01N NaOH 64 mL<br />
Distilled water 36 mL<br />
1. Dissolve the Bromothymol Blue in the NaOH<br />
2. Add to the water.<br />
To prepare medium (1 litre for plates):<br />
SPECIALISED CULTURE MEDIA<br />
Distilled water 980 mL Solution B 20 mL<br />
Bacto Agar (BD 214010) 20 g<br />
1. Autoclave to 121 O C for 15 minutes, cool to 48 O C.<br />
2. For plates add 100 mL of the filtered solution A and mix. Dispense in<br />
plates.
Descriptions of Medical Fungi 183<br />
SPECIALISED CULTURE MEDIA<br />
Cornmeal Agar.<br />
for routine cultivation and identification of fungi.<br />
Cornmeal agar (Oxoid CM 0103) 8.5 g<br />
Distilled water 500 mL<br />
1. Mix dry ingredients into 100 mL H 2 O, boil remaining water.<br />
2. Add boiling water to mixture and bring to boil.<br />
3. Autoclave for 10 minutes at 120 O C, then slope on racks.<br />
Cornmeal Glucose Sucrose Yeast Extract Agar.<br />
for zygomycete sporulation<br />
Cornmeal agar (Oxoid CM 0103) 17 g<br />
Dextrose (Glucose) 2 g<br />
Sucrose 3 g<br />
Yeast extract 1 g<br />
Distilled water 1000 mL<br />
1. Mix dry ingredients into 100 mL H 2 O, boil remaining water.<br />
2. Add boiling water to mixture and bring to boil.<br />
3. Dispense for slopes.<br />
4. Autoclave for 10 minutes at 120 O C, remove and slope.<br />
Czapek Dox Agar.<br />
for routine cultivation of fungi, especially Aspergillus, Penicillium,<br />
and non-sporulating moulds.<br />
Czapek Dox Agar (Oxoid CM97) 45.4 g<br />
Distilled water 1000 mL<br />
1. Soak the ingredients in small amount of water.<br />
2. Bring remaining water to boil, add to soaking ingredients and bring to<br />
the boil again, stirring continuously.<br />
3. Dispense for slopes as required.<br />
4. Autoclave at 121 O C for 10 minutes, remove and slope or pour for plates<br />
as required.<br />
Dixon’s Agar (modified).<br />
for primary isolation and cultivation of Malassezia species.<br />
Malt extract (Oxoid L39) 9 g Bacto Tryptone 1.5 g<br />
Ox-bile Desiccated (Oxoid L50) 5 g Tween 40 2.5 mL<br />
Oleic acid 0.5 g Glycerol 0.5 mL<br />
Bacto Agar 3 g Distilled water 250 mL<br />
1. Soak ingredients in a little of the water.<br />
2. Bring remaining water to boil, add to the soaking ingredients and bring<br />
to the boil again constantly stirring.<br />
3. Dispense for slopes (7 mL amounts into 30 mL disposable bottles.<br />
4. Autoclave at 121 O C for 10 minutes and then slope.
184<br />
Descriptions of Medical Fungi<br />
SPECIALISED CULTURE MEDIA<br />
Hair Perforation Test.<br />
for the differentiation of Trichophyton species.<br />
Blonde pre-pubital hair cut into short pieces (1 cm) 10-20 hairs<br />
Distilled water 5 mL<br />
1. Autoclave hair at 121 O C for 10 minutes and store in sterile container.<br />
2. Place 10-20 short pieces of hair in 5 mL water in vial.<br />
3. Inoculate with small fragments of the test fungus.<br />
4. Incubate at room temperature.<br />
5. Individual hairs are removed at intervals up to 4 weeks and examined<br />
microscopically in lactophenol cotton blue. Isolates of T. mentagrophytes<br />
produce marked localised areas of pitting and marked erosion whereas<br />
those of T. rubrum do not.<br />
Lactritmel Agar.<br />
for the production of pigment by Trichophyton species.<br />
Skimmed milk powder<br />
7 g<br />
(use only Dutch Jug skimmed milk powder)<br />
Honey 10 g<br />
Cornmeal agar (Oxoid CM 0103) 17 g<br />
Chloramphenicol 1 x 250 capsule<br />
Distilled water 1000 mL<br />
1. Weigh skimmed milk into stainless steel jug. Slowly add some water,<br />
mixing milk into smooth paste. Continue adding small quantities of<br />
water until powder is dissolved (about 150 mL).<br />
2. Weigh other ingredients into skimmed milk and allow to soak.<br />
3. Boil remaining water, and with it wash out honey from beaker.<br />
4. Add to other ingredients and boil.<br />
5. Dispense for slopes (7 mL).<br />
6. Autoclave for 10 minutes at 115OC. 7. On removal from autoclave allow to stand 5 minutes then shake and<br />
slope on racks.<br />
Note: Do not filter or adjust pH in any way<br />
Littman Oxgall Agar.<br />
for the differentiation of Trichophyton species.<br />
Littman Oxgall Agar (US Biological L3025) 27.5 g<br />
Distilled water 500 mL<br />
1. Soak agar in 100 mL of water in stainless steel jug. Boil remaining<br />
400mL in a separate jug.<br />
2. When water has boiled add to soaking agar and reboil, stirring<br />
constantly.<br />
3. Dispense for slopes.<br />
4. Autoclave for 10 minutes at 121 O C, remove and slope.
Descriptions of Medical Fungi 185<br />
SPECIALISED CULTURE MEDIA<br />
Malt Extract Agar.<br />
for routine cultivation and identification of fungi.<br />
Oxoid Malt Extract (L39) 20 g<br />
Bacto Agar (BD 214010) 20 g<br />
Distilled water 1000 mL<br />
1. Dissolve malt extract in a plastic beaker and pH the solution to pH 6.5<br />
with NaOH.<br />
2. Soak agar in small quantity of solution. Bring remaining solution to<br />
the boil, stirring constantly.<br />
3. Add to soaking agar. Bring to boil, stirring constantly.<br />
4. Dispense for slopes as required.<br />
5. Autoclave at 121 O C for 10 minutes, remove and slope or pour for<br />
plates as required.<br />
1% Peptone Agar.<br />
for the differentiation of Trichophyton species.<br />
Tryptone Peptone (BD 211705) 5 g<br />
Bacto Agar (BD 214010) 10 g<br />
Distilled water 500 mL<br />
1. Soak agar and peptone in about 50 mL of water.<br />
2. Boil remaining water, add this to soaking ingredients and bring to boil<br />
again.<br />
3. Dispense for slopes (7 mL).<br />
4. Autoclave for 10 minutes at 121 O C, then slope on racks.<br />
Potato Dextrose Agar.<br />
for routine cultivation and identification of fungi.<br />
Potato Dextrose Agar (Oxoid CM139) 39 g<br />
Distilled water 1000 mL<br />
1. Soak potato dextrose agar in small amount of the water in a stainless<br />
steel jug.<br />
2. Boil remaining water, add to soaking ingredients, bring to the boil,<br />
stirring constantly.<br />
3. Dispense for slopes as required.<br />
4. Autoclave at 121 O C for 15 minutes. Remove and slope or pour for<br />
plates as required.<br />
Rice Grain Slopes.<br />
to induce sporulation and for differentiation of M. audouinii and M. canis.<br />
Polished rice grains Distilled water<br />
1. Place ~ 1/2 teaspoon rice grains into wide neck 20 mL glass vials.<br />
2. Add 8 mL distilled water to each vial.<br />
3. Lid, then slope on racks ensuring rice grains are evenly distributed.<br />
4. Autoclave racks at 121 O C for 15 minutes.
186<br />
Descriptions of Medical Fungi<br />
SPECIALISED CULTURE MEDIA<br />
Sabouraud Dextrose Agar with Cycloheximide, Chloramphenicol,<br />
Gentamicin and Yeast Extract.<br />
for the primary isolation and cultivation of dermatophytes.<br />
Sabouraud Dextrose Agar (Oxoid CM41) 65 g<br />
Cycloheximide (Actidione) 0.5 g<br />
Chloramphenicol 1 x 250 capsule<br />
Gentamicin (40mg/mL) 0.56 mL<br />
Yeast extract 5 g<br />
Distilled water 1000 mL<br />
1. Soak all ingredients, except Gentamicin, in 100 mL water.<br />
2. Boil remaining water, add to soaking ingredients, and bring to boil to<br />
dissolve, stirring well to prevent from charring.<br />
3. Add the Gentamicin. Mix well.<br />
4. Dispense for slopes as required.<br />
5. Autoclave at 121 O C for 10 minutes. Remove and slope, or pour for plates<br />
as required.<br />
Sabouraud Dextrose Agar with Chloramphenicol and Gentamicin.<br />
for primary isolation and routine culture of yeasts and moulds.<br />
Sabouraud Dextrose Agar (Oxoid CM41) 65 g<br />
Chloramphenicol 1 x 250 capsule<br />
Gentamicin (40mg/mL) 0.56 mL<br />
Distilled water 1000 mL<br />
See above method for Sabouraud Dextrose Agar with Cycloheximide,<br />
Chloramphenicol, Gentamicin and Yeast Extract.<br />
Sabouraud Dextrose Agar with 5% Salt.<br />
for the differentiation of Trichophyton species.<br />
Sabouraud Dextrose Agar (Oxoid CM41) 32.5 g<br />
Sodium Chloride NaCl (Univar 465) 25 g<br />
Distilled water 500 mL<br />
1. Soak ingredients in approximately 100 mL water.<br />
2. Bring remaining water to boil, add to soaking ingredients.<br />
3. Dispense for slopes (7 mL).<br />
4. Autoclave at 118 O C for 10 minutes, then slope on racks.
Descriptions of Medical Fungi 187<br />
Tap Water Agar.<br />
for the stimulation of sporulation in Apophysomyces and Saksenaea isolates.<br />
Bacto Agar (BD 214010) 15 g<br />
Distilled water 1000 mL<br />
1. Add agar to water in stainless steel jug, allow to soak.<br />
2. Dispense for slopes.<br />
3. Autoclave at 118 O C for 10 minutes, remove and slope.<br />
Urease Agar Slopes with 0.5% Glucose.<br />
for the differentiation of Urease producing organisms.<br />
Urease glucose broth base:<br />
Urea, broth base (Oxoid CM71) 0.9 g<br />
Glucose 5 g<br />
Distilled water 450 mL<br />
1. Add the Urea broth base and glucose to the distilled water in a 500mL<br />
beaker.<br />
2. Dispense in 5 X 90 mL amounts.<br />
3. Autoclave at 115 O C for 20 mins.<br />
4. When cool, label and store in the fridge.<br />
Method to make slopes:<br />
SPECIALISED CULTURE MEDIA<br />
40% Urea Solution (Oxoid SR 20) 10 mL<br />
Bacto Agar (BD 214010) 3 g<br />
Distilled water 100 mL<br />
1. Add 3.0 grams of agar to 100 mL of distilled water in a 250 mL pyrex<br />
bottle.<br />
2. Autoclave at 121 O C for 15 minutes and place in 50 O C water bath.<br />
3. When cool add 90 mL of the Urease broth with glucose and the 10 mL<br />
of 40% urea solution to agar and dispense in 3 mL aliquots and slope<br />
on racks.<br />
Vitamin Free Agar (Trichophyton Agar No.1).<br />
for the differentiation of Trichophyton species.<br />
Trichophyton Agar No. 1 (BD 287710) 11.8 g<br />
Distilled water 200 mL<br />
1. Add agar to water in stainless steel jug, allow to soak.<br />
2. Bring to boil to dissolve, stirring constantly.<br />
3. Once boiled remove immediately to avoid discolouration.<br />
4. Dispense for slopes.<br />
5. Autoclave at 118 O C for 10 minutes, remove and slope.
188<br />
Descriptions of Medical Fungi<br />
REFERENCES<br />
Adam, R.D., M.L. Paquin, E.A. Petersen et al. (1986). Phaeohyphomycosis caused<br />
by the fungal genera Bipolaris and Exserohilum. A report of 9 cases and review of<br />
the literature. Medicine. 65:203-217.<br />
Ajello, L. 1957. Coccidioides immitis: Isolation procedures and diagnostic criteria.<br />
Proceedings of symposium on Coccidioidomycosis. Public Health Publication No.<br />
575, CDC Atlanta, USA.<br />
Ajello, L. 1977. Taxonomy of the dermatophytes: a review of their imperfect and perfect<br />
states. In “Recent Advances in Medical and Veterinary Mycology” (K. Iwata,<br />
ed.), pp. 289-297. University Park Press, Baltimore, Maryland, USA.<br />
Ajello, L., D.F. Dean and R.S. Irwin. 1976. The zygomycete Saksenaea vasiformis<br />
as a pathogen of humans with a critical review of the etiology of zygomycosis. Mycologia.<br />
68:52-62.<br />
Alcorn, J.L. 1983. Genetic concepts in Drechslera, Bipolaris and Exserohilum. Mycotaxon.<br />
17:1-86.<br />
Al-Mohsen, I.Z., D.A. Sutton, L. Sigler et. al. 2000. Acrophialophora fusispora brain<br />
abscess in a child with acute lymphoblastic leukaemia: review of cases and taxonomy.<br />
J. Clin. Microbiol. 38:4569-4576.<br />
Alvarado-Ramirez, E., J.M. Torres-Rodriguez. 2007. In vitro susceptibility of Sporothrix<br />
schenckii to six antifungal agents using three different methods. Antimicrob.<br />
Agents Chemother. Apr 16 (Epub).<br />
Ames, L.M. 1963. A monograph of the Chaetomiaceae. U.S. Army Research and<br />
Development Serial. 2:1-125.<br />
Barnett, J.A., R.W. Payne and D. Yarrow. 1983. Yeasts: characteristics and identification.<br />
Cambridge University Press, London, UK.<br />
Barron, G.L. 1968. The genera of hyphomycetes from soil. Williams & Wilkins Co.<br />
Balitmore, USA.<br />
Booth, C. 1966. The genus Cylindrocarpon. Mycol. Pap. 104:1-56.<br />
Booth, C. 1971. The genus Fusarium. Commonwealth Mycological Institute, Kew,<br />
Surrey, England.<br />
Booth, C. 1977. Fusarium: laboratory guide to the identification of the major species.<br />
Commonwealth Mycological Institute, Kew, Surrey, England.<br />
Buchta, V. and M. Otcenasek. 1988. Geotrichum candidum - an opportunistic agent<br />
of mycotic diseases. Mycoses. 31:363-370.<br />
Burges, G.E., C.T. Walls and J.C. Maize. 1987. Subcutaneous phaeohyphomycosis<br />
caused by Exserohilum rostratum in an immunocompetent host. Arch. Dermatol.<br />
123:1346-1350.<br />
Burgess, L.W. and C.M. Liddell. 1983. Laboratory manual for Fusarium research.<br />
Fusarium Research Laboratory, Department of Plant Pathology and Agricultural<br />
Entomology. The University of Sydney.<br />
Campbell, C.K. and M.D. Smith. 1982. Conidiogenesis in Petriellidium boydii (Pseudallescheria<br />
boydii). Mycopathologia. 78:145-150.<br />
Carmichael, J.W. 1962. Chrysosporium and some aleuriosporic hyphomycetes. Can.<br />
J. Bot. 40:1137-1173.<br />
Casadevall, A. and J.R. Perfect. 1988. Cryptococcus neoformans. ASM Press<br />
USA.<br />
Catanzaro, A. 1985. Coccidiomycosis. In Fungal Diseases of the Lung, eds G.A.<br />
Sarosi and S.F. Davies. Grune and Stratton Inc.<br />
Cavalier-Smith, T. 1998. A revised six-kingdom system of life. Biol Rev Canm Philos<br />
Soc. 73: 203-266.
Descriptions of Medical Fungi 189<br />
REFERENCES<br />
Chandler, F.W., W. Kaplan and L. Ajello. 1980. A colour atlas and textbook of the<br />
histopathology of mycotic diseases. Wolfe Medical Publications Ltd.<br />
Cooney, D.H. and R. Emerson. 1964. Thermophilic fungi. W.H. Freeman & Co.<br />
Cooter, R.T., I.S. Lim, D.H. Ellis et. al. 1990. Burn wound zygomycosis caused by<br />
Apophysomyces elegans. J.Clin. Microbiol. 28: 2151-2153.<br />
Cuenca-Estrella, M., A. Gomez-Lopez, E. Mellado et. al. 2006. Head-to head comparision<br />
of the activities of currently available antifungal agents against 3,378 Spanish<br />
clinical isolates of yeasts and filamentous fungi. Antimicrob. Agents Chemother.<br />
50:917-921.<br />
Dannaoui, E., J. Meletiadis, J.W. Mouton et. al. 2003. In vitro susceptibilities of zygomycetes<br />
to conventional and new antifungals. J. Antimicrob. Chemother. 51:45-<br />
52.<br />
Davis, S.R., D.H. Ellis, P. Goldwater et. al. 1994. First human culture-proven Australian<br />
case of entomophthoromycosis caused by Basidiobolus ranarum. J Med.<br />
Vet. Mycol. 32: 225-230.<br />
de Hoog, de G.S. 1972. The genera Beauvaria, Isaria, Tritrachium and Acrodontium<br />
Gen. Nov. Studies in Mycology, Centraalbureau voor Schimmelcultures, Baarn.<br />
1:1-41.<br />
de Hoog, G.S. 1977. Rhinocladiella and allied genera. Studies in Mycology, Centraalbureau<br />
voor Schimmelcultures, Baarn. 15:1-140<br />
de Hoog, G.S. 1983. On the potentially pathogenic dematiaceous Hyphomycetes. In:<br />
D.H. Howard (ed). The fungi pathogenic to humans and animals. A:149-216.<br />
de Hoog, G.S. 1985. The taxonomic structure of Exophiala. in Fungi pathogenic for<br />
humans and animals. Part B: Pathogenicity and detection: II. (ed. D. Howard).<br />
Marcel Dekker Inc.<br />
de Hoog, G.S., E. Gueho, F. Masclaux et. al. 1995. Nutritional physiology and<br />
taxonomy of human-pathogenic Cladosporium-Xylohypha species. J. Med. Vet.<br />
Mycol. 33:339-347.<br />
de Hoog, G.S. and E.J. Hermanides-Nijhof. 1977. The black yeasts and allied hyphomycetes.<br />
Studies in Mycology No. 15. Centraalbureau voor Schimmelcultures,<br />
The Netherlands.<br />
de Hoog, G.S., A.H. Rantio-Lehtimaki and M.TH. Smith. 1985. Blastobotryis; Sporothrix<br />
and Trichosporiella; generic delimitation, new species, and a Stephanoascus<br />
teleomorph. Antontie van Leeuwenhoek. 51:79-109.<br />
de Hoog, G.S., V. Vincent, R.B. Caligiorne et. al. 2003. Species diversity and polymorphism<br />
in the Exophiala spinifera clade containing opportunistic black yeastslike<br />
fungi. J. Clin. Microbiol. 41:4767-4778.<br />
de Hoog, G.S., D. Attili, V.A. Vicente et. al. 2004. Molecular ecology and pathogenic<br />
potential of Fonsecaea species. Med. Mycol. 42:405-416.<br />
de Hoog, G.S., J. Guarro, J. Gene and M.J. Figueras. 2000. Atlas of Clinical Fungi<br />
(second edition). Centraalbureau voor Schimmelcultures, Utrecht, The Netherlands.<br />
de Hoog, G.S., J.S. Zeng, M.J. Harrak and D.A. Sutton. 2006. Exophiala xenobiotica<br />
sp. nov., an opportunistic black yeast inhabiting environments rich in hydrocarbons.<br />
Antonie Van Leeuwenhoek 90:257-268.<br />
Diekema, D.J., S.A. Messer, R.J. Hollis et. al. 2003. Activities of caspofungin, itraconazole,<br />
posaconazole, ravuconazole, voriconazole, and amphotericin B against<br />
448 recent clinical isolates of filamentous fungi. J. Clin. Microbiol. 41:3623-3626.
190<br />
Descriptions of Medical Fungi<br />
REFERENCES<br />
Dixon, D.M. and A. Polak-Wyss. 1991. The medically important dematiaceous fungi<br />
and their identification. Mycoses. 34:1-18.<br />
Domsch, K.H., W. Gams and T.H. Anderson. 1980. Compendium of soil fungi. Volume<br />
1. Academic Press.<br />
Dworzack, D.L., A.S. Pollock, G.L. Hodges et. al. 1978. Zygomycosis of the maxillary<br />
sinus and palate caused by Basidiobolus haptosporus. Arch. Intern. Med.<br />
138:1274-1276<br />
Ellis, D.H. 1981. Ascocarp morphology and terminal hair ornamentation in thermophilic<br />
Chaetomium species. Mycologia. 73:755-773.<br />
Ellis, D.H. 2005a. Subcutaneous Zygomycetes - Entomophthoromycosis. Chapter<br />
17. In Topley and Wilson’s Microbiology and Microbial Infections: medical Mycology,<br />
10th edition, Hodder Arnold London. pp 347-355.<br />
Ellis, D.H. 2005b. Systemic Zygomycetes - Mucormycosis. Chapter 33. In Topley<br />
and Wilson’s Microbiology and Microbial Infections: Medical Mycology, 10th edition,<br />
Hodder Arnold London. pp 659-686.<br />
Ellis, D.H., and G. Kaminski 1984. Laboratory identification of Saksenaea vasiformis:<br />
a rare cause of zygomycosis in Australia. Sabouraudia: Journal of Medical<br />
and Veterinary Mycology. 23:137-140.<br />
Ellis, D.H., and P.J. Keane. 1981. Thermophilic fungi isolated from some Australian<br />
soils. Aust. J. Bot. 29:689-704.<br />
Ellis, J.J. 1985. Species and varieties in Rhizopus arrhizus - Rhizopus oryzae group<br />
as indicated by their DNA complementarity. Mycologia. 77:243-247.<br />
Ellis, J.J. 1986. Species and varieties in the Rhizopus microsporus group as indicated<br />
by their DNA complementarity. Mycologia. 78:508-510<br />
Ellis, J.J., and L. Ajello. 1982. An unusual source of Aphophysomyces elegans and<br />
a method of stimulating sporulation of Saksenaea vasiformis. Mycologia 74:144-<br />
145.<br />
Ellis, J.J. and C.W. Hesseltine. 1966. Two new families of Mucorales. Mycologia.<br />
66:87-95.<br />
Ellis, J.J. and C.W. Hesseltine. 1965. The genus Absidia: globose spored species.<br />
Mycologia. 57:222-235.<br />
Ellis, J.J. and C.W. Hesseltine. 1966. Species of Absidia with ovoid sporangiospores.<br />
II. Sabouraudia. 5:59-77.<br />
Ellis, M.B. 1971. Dematiaceous Hyphomycetes. Commonwealth Mycological Institute,<br />
Kew, Surrey, England.<br />
Ellis, M.B. 1976. More Dematiaceous Hyphomycetes. Commonwealth Mycological<br />
Institute, Kew, Surrey, England.<br />
Emmons, C.W. and C.H. Bridges. 1977. Entomophthora coronata, the etiologic<br />
agent of a phycomycosis of horses. Mycologia. 53:307-312.<br />
Espinel-Ingroff, A., K. Boyle and D.J. Sheehan. 2001. In vitro antifungal activities<br />
of voriconazole and reference agents as determined by NCCLS methods: review of<br />
the literature. Mycopathologia 150:101-115.<br />
Espinel-Ingroff, A. 2001. In vitro fungicidal activities of voriconazole. itraconazole.<br />
and amphotericin B against opportunistic moniliaceous and dematiaceous fungi. J.<br />
Clin. Microbiol. 39:954-958.<br />
Espinel-Ingroff, A. 2003. In vitro antifungal activities of anidulafungin and micrafungin,<br />
licensed agents and the investigational triazole posaconazole as determined by<br />
NCCLS methods for 12,052 fungal isolates: review of the literature. Rev. Iberoam.<br />
Micol. 20:121-136.
Descriptions of Medical Fungi 191<br />
REFERENCES<br />
Espinel-Ingroff, A. 2006. Comparison of three commercial assays and a modified<br />
disk diffusion assay with two broth microdilution reference assays for testing zygomycetes,<br />
Aspergillus spp., Candida spp., and Cryptococcus neoformans with<br />
posaconazole and amphotericin B. J. Clin. Microbiol. 44:3616-3622.<br />
Fernandez-Torres, B., A.J. Carrillo, E. Martin et al. 2001. In vitro activities of 10<br />
antifungal drugs against 508 dermatophyte strains. Antimicrob. Agents Chemother.<br />
45:2524-2528.<br />
Ferry, A.P. and S. Abedi. 1983. Diagnosis and management of rhino-orbitocerebral<br />
mucormycosis (phycomycosis). Ophathalmology. 90: 1096-1104.<br />
Fisher, M.C., G.L. Koenig, T.J. White and J.W. Taylor. 2002. Molecular and phenotypic<br />
description of Coccidioides posadasii sp. nov., previously recognised as the<br />
non-California population of Coccidioides immitis. Mycologia. 94:73-84.<br />
Frankel, D.H. and J.W. Rippon. 1989. Hendersonula toruloidea infection in man.<br />
Mycopathologia. 105:175-186.<br />
Franzot, S.P., I.R. Salkin and A. Casadevall. 1999. Cryptococcus neoformans var.<br />
grubii: separate varietal status for Cryptococcus neoformans serotype A isolates.<br />
J. Clin. Microbiol. 37:838-840.<br />
Frye, C.B. and J. Reinhardt. 1993. Characterization of groups of the zygomycete<br />
genus Rhizopus. Mycopathologia. 124: 139-147.<br />
Gams, W. 1971. Cephalosporium-artige Schimmelpilze (Hyphomycetes). G. Fisher,<br />
Stuttgart, p.262.<br />
George, R.B. and R.L. Penn. 1986. Histoplasmosis. In Fungal diseases of the Lung.<br />
eds Sarosi, G.A. and S.F. Davies. Grune and Stratton Inc.<br />
Gilgado, F., J. Cano, J. Gene and J. Guarro. 2005. Molecular phylogeny of the<br />
Pseudallescheria boydii species complex: proposal of two new species. J. Clin.<br />
Microbiol. 43:4930-4942.<br />
Girmenia, C., G. Pizzarelli, D. D’Antonio et. al. 2003. In vitro susceptibility testing of<br />
Geotrichum capitatum: comparison of the Etest, disk diffusion, and sensititre colorimetric<br />
methods with the NCCLS M27-A2 broth microdilution reference method.<br />
Antimicrob. Agents Chemother. 47:3985-3988.<br />
Goldschmied-Reouven, A., A. Shvoron, M. Topaz and C. Block. 1989. Saksenaea<br />
vasiformis infection in a burn wound. J. Med. Vet. Mycol. 27:427-429.<br />
Gonzalez G.M., A.W. Fothergill, D.A. Sutton et al. 2005. In vitro activities of new<br />
and established triazoles against opportunistic filamentous and dimorphic fungi.<br />
Med. Mycol. 43:281-284.<br />
Goodman, N.L. and M.G. Rinaldi. 1991 Agents of zygomycosis. In Balows, A., Hausler,<br />
W.J., Herrmann, K.L. et al. (eds.), Manual Clinical Microbiology 5th edition.<br />
American Society for Microbiology Washington DC.<br />
Graser, Y., S. de Hoog and R.C. Summerbell. 2006. Dermatophytes: recognising<br />
species of clonal fungi. Med. Mycol. 44:199-209.<br />
Greer, D.L. and L. Friedman. 1966. Studies on the genus Basidiobolus with reclassification<br />
of the species pathogenic for man. Sabouraudia. 4:231-241.<br />
Guarro, J., W. Gams, I. Puiol and J. Gene. 1997. Acremonium species: new emerging<br />
fungal opportunistics: in vitro antifungal susceptibilities and review. Clin. Infect.<br />
Dis. 25:1222-1229.<br />
Gueho, E.S. 1979. Dexoyribonucleic acid base composition and taxonomy in the<br />
genus Geotrichum Link. Antonie van Leeuwenhoek. 45:199-210.<br />
Gueho, E. and G.S. de Hoog. 1991. Taxonomy of the medical species of Pseudallescheria<br />
and Scedosporium. J. Mycol. Med. 118:3-9.
192<br />
Descriptions of Medical Fungi<br />
REFERENCES<br />
Gueho, E., M.Th. Smith, G.S. de Hoog et. al. 1992. Contributions to a revision of the<br />
genus Trichosporon. Antonie van Leeuwenhoek. 61:289-316.<br />
Gueho, E., G. Midgley and J. Guillot. 1996. The genus Malassezia with description<br />
of four new species. Antonie Van Leeuwenhoek. 69:337-55.<br />
Guillot J. and E. Gueho. 1995. The diversity of Malassezia yeasts confirmed by rRNA<br />
sequence and nuclear DNA comparisons. Antonie Van Leeuwenhoek. 67:297-<br />
314.<br />
Guillot J., E. Gueho, M. Lesourd et al. 1996. Identification of Malassezia species.<br />
J. Mycol. Med. 6:103-110.<br />
Guillot J., M. Deville, M. Berthelemy et. al. 2000. A single PCR-restriction endonuclease<br />
analysis for rapid identification of Malassezia species. Lett. Appl. Microbiol.<br />
31:400-403.<br />
Gupta, A.K., C.B. Horgan-Bell and R.C. Summerbell. 1998. Onychomycosis associated<br />
with Onychocola canadensis: ten case reports and a review of the literature.<br />
J. A. Acad. Dermatol. 39:410-407.<br />
Hajjeh, R.A., A.N. Sofair, L.H. Harrison et. al. 2004. Incidence of bloodstream infections<br />
due to Candida species and in vitro susceptibilities of isolates collected from<br />
1998 to 2000 in a population based active surveillance program. J. Clin. Microbiol.<br />
42:1519-1527.<br />
Hermanides-Nijhof, E.J. 1977. Aureobasidium and allied genera. Studies in Mycology,<br />
Baarn. 15:141-177.<br />
Hesseltine, C.W. and J.J. Ellis. 1964. The genus Absidia: Gongronella and cylindrical-spored<br />
species of Absidia. Mycologia. 56:568-601.<br />
Hesseltine, C.W. and J.J. Ellis. 1964. An interesting case of Mucor, M. ramosissimus.<br />
Sabouraudia. 3: 151-154.<br />
Hesseltine, C.W. and J.J. Ellis. 1966. Species of Absidia with ovoid sporangiospores.<br />
I. Mycologia. 58:173-194.<br />
Hohl, P.E., H.P. Holley, E. Prevost et. al. 1983. Infections due to Wangiella dermatitidis<br />
in humans: Report of the first documented case from the United States and a<br />
review of the literature. Reviews of Infectious Diseases. 5:854-864.<br />
Holland, J. 1997. Emerging zygomycosis of humans: Saksenaea vasiformis and<br />
Apophysomyces elegans. Curr. Top. Med. Mycol. 8: 27-34.<br />
Humber, R.A., C.C. Brown and R.W. Kornegay. 1989. Equine zygomycosis caused<br />
by Conidiobolus lampragues. J. Clin. Microbiol. 27: 573–6.<br />
Irokanulo, E.A.O., C.O. Akueshi and A.A. Makinde. 1994. Differentiation of Cryptococcus<br />
neoformans serotypes A and D using creatinine dextrose bromothymol blue<br />
thymine medium. Br. J. Biomed. Sci. 51:100-103.<br />
Jong, S.C. and F.M. Dugan. 2003. Zygomycetes: The Order Entomophthorales. In<br />
Howard, D.H. (ed.), Pathogenic Fungi in Humans and Animals. 2 nd edition, Marcel<br />
Dekker Inc., New York, 127-139.<br />
Kane, J., R. Summerbell, L. Sigler et. al. 1997. Laboratory handbook of dermatophytes.<br />
Star Publishing Co. Belmont, CA. USA.<br />
Kaplan, W. 1977. Protothecosis and infections caused by morphologically similar<br />
green algae. The black and white yeasts. Proceedings of the Fourth International<br />
Conference on the Mycoses. Scientific Publication No. 356. Pan American Health<br />
Organization. Washington D.C. USA.<br />
Kaufman, L. and P.G. Standard. 1987. Specific and rapid identification of medically<br />
important fungi by exoantigen detection. Ann. Rev. Microbiol. 41:209-225.
Descriptions of Medical Fungi 193<br />
REFERENCES<br />
Kerr, P.G., H. Turner, A. Davidson et. al. 1988. Zygomycosis requiring amputation<br />
of the hand: an isolated case in a patient receiving haemodialysis. Med. J. Aust.<br />
148: 258-259.<br />
Khan, Z.U., N.A. Al-Sweih, S. Ahmad et. al. 2007. Outbreak of fungemia among<br />
neonates caused by Candida haemulonii resistant to amphotericin B, itraconazole,<br />
and fluconazole. J. Clin. Microbiol. 45:2025-2027.<br />
King, D.S. 1976a. Systematics of Conidiobolus (Entomophthorales) using numerical<br />
taxonomy. I. Biology and cluster analysis. Can J Bot 54: 45-46.<br />
King, D.S. 1976b. Systematics of Conidiobolus (Entomophthorales) using numerical<br />
taxonomy. II. Taxonomic considerations. Can J Bot 54: 1285-1296.<br />
King, D.S. 1983. Entomophthorales. In: Howard DH, ed. Fungi pathogenic for humans<br />
and animals. Part A Biology. Marcel Dekker Inc. New York pp 61-73.<br />
Klich, M.A. 2002. Identification of common Aspergillus species. Centraalbureau voor<br />
Schimmelcultures, The Netherlands.<br />
Kreger-van Rij, N.J.W. (ed.). 1984. The yeasts, a taxonomic study, 3 rd edition. Elsevier<br />
Sci. Publ., Amsterdam, 1082 pp.<br />
Kucukates, E., Z. Erturan, S. Susever and Y. Yegenoglu. 2005. In vitro susceptibility<br />
of yeast isolated from patients in intensive care units to fluconazole and amphotericin<br />
B during a 3-year period. APMIS 113:278-283.<br />
Kurtzman and J.W. Fell. 1998. The Yeasts: a taxonomic study. 4 th Edition. Elsevier<br />
Science Publishers B.V. Amsterdam.<br />
Kwon-Chung K.J., Polacheck I. and Bennett J.E. (1982): Improved diagnostic medium<br />
for separation of Cryptococcus neoformans var. neoformans Serotypes A and<br />
D) and Cryptococcus neoformans var. gattii (Serotypes B and C). – J. Clin. Microbiol.<br />
15:535-537.<br />
Kwon-Chung, K.J. and J.W. Bennett. 1992. Medical Mycology. Lea & Febiger,<br />
Philadelphia, 861pp.<br />
Lawrence, R.M., Snodgrass, W.T., Reichel, G.W. et. al. 1986. Systemic zygomycosis<br />
caused by Apophysomyces elegans. J. Med. Vet. Mycol. 24: 57-65.<br />
Lunn, J.A. and W.A. Shipton. 1983. Re-evaluation of taxonomic criteria in Cunninghamella.<br />
Trans. Br. Mycol. Soc. 81:303-312.<br />
Luttrell, E.S. 1978. Biosystematics of Helminthosporium: impact on agriculture. In<br />
Biosystematics in Agriculture. eds. J.A. Romberger et al. Allanheld, Osmon & Co.,<br />
N.J. USA.<br />
Mackenzie, D.W.R., W. Loeffler, A. Mantovani and T. Fujikura. 1986. Guidelines for<br />
the prevention, preservation and control of dermatophytoses in man and animals.<br />
World Health Organization.<br />
Malloch, D. and I.F. Salkin. (1984). A new species of Scedosporium associated with<br />
osteomyelitis in humans. Mycotaxon. 21:247-255.<br />
Matsumoto, T., A.A. Padhye and L. Ajello. 1987. Medical significance of the socalled<br />
black yeasts. Eur. J. Epidemiol. 3:87-95.<br />
Matsumoto, T., A.A. Padhye, L. Ajello et. al. 1984. Critical review of human isolates<br />
of Wangiella dermatitidis. Mycologia. 76:232-249.<br />
McGinnis, M.R. 1978. Human pathogenic species of Exophiala, Phialophora, and<br />
Wangiella. In the black and white yeasts. Proceedings of the fourth international<br />
conference on the mycoses. 1978. Scientific Publication No. 356. Pan American<br />
Health Organization. Washington D.C. USA. pp.37-59.<br />
McGinnis, M.R. 1978. Taxonomy of Exophiala jeanselmei. Mycopathologia. 65:79-<br />
87.
194<br />
Descriptions of Medical Fungi<br />
REFERENCES<br />
McGinnis, M.R. 1980. Laboratory handbook of medical mycology. Academic Press.<br />
McGinnis, M.R. and D. Borelli. 1981. Cladosporium bantianum and its synonym<br />
Cladosporium trichoides. Mycotaxon. 13:127-136.<br />
McGinnis, M.R. and W.A. Schell and J. Carson. 1985. Phaeoannellomyces and<br />
the Phaeococcomycetaceae, new dematiaceous blastomycete taxa. J. Med. Vet.<br />
Mycol. 23:179-188.<br />
McGinnis, M.R., D. Borelli, A.A. Padhye and L. Ajello. 1986a. Reclassification of<br />
Cladosporium bantiana in the genus Xylohypha. J. Clin. Microbiol. 23:1148-1151.<br />
McGinnis, M.R., M.G. Rinaldi and R.E. Winn. 1986b. Emerging agents of Phaeohyphomycosis:<br />
pathogenic species of Bipolaris and Exserohilum. J. Clin. Microbiol.<br />
24:250-259.<br />
McGinnis, M.R. and A.A. Padhye. 1977. Exophiala jeanselmei, a new combination<br />
for Phialophora jeanselmei. Mycotaxon. 5:341-352.<br />
McGinnis, M.R., A.A. Padhye and L. Ajello. 1982. Pseudallescheria Negroni et<br />
Fischer, 1943 and its later synonym Petriellidium Malloch, 1970. Mycotaxon 9:94-<br />
102.<br />
McGinnis, M.R., N. Nordoff, R.K. Li et. al. 2001. Sporothrix schenckii sensitivity to<br />
voriconazole, itraconazole and amphotericin B. Med. Mycol. 39:369-371.<br />
McGinnis, M.R. and L. Pasarell. 1998. In vitro testing of susceptibilities of filamentous<br />
ascomycetes to voriconazole, itraconazole, and amphotericin B, with consideration<br />
of phylogenetic implications. J. Clin. Microbiol. 36:2353-2355.<br />
Metin, D.Y., S. Hilmioglu-Polat, F. Hakim et. al. 2005. Evaluation of the microdilution,<br />
Etest and disk diffusion methods for antifungal susceptibility testing of clinical<br />
strains of Trichosporon spp. J. Chemother. 17:404-408.<br />
Millner, P.D. 1975. Radial growth responses to temperature by 58 Chaetomium species,<br />
and some taxonomic relationships. Mycologia. 69:492-502.<br />
Miranda, K.C., C.R. de Araujo, C.R. Costa et. al. 2007. Antifungal activities of azole<br />
agents against the Malassezia species. Int. J. Antimicrob. Agents. 29:281-284.<br />
Misra, P.C., Srivastava, K.J. and Latas, K. 1979. Apophysomyces, a new genus of<br />
the Mucorales. Mycotaxon. 8: 377-382.<br />
Mok, W.Y. 1982. Nature and identification of Exophiala werneckii. J. Clin. Microbiol.<br />
16:976-978.<br />
Montel, E., P.D. Bridge and B.C. Sutton. 1991. An integrated approach to Phoma<br />
systematics. Mycopathologia. 115:89-103.<br />
Moore, M.K. 1986. Hendersonula toruloidea and Scytalidium hyalinum infections in<br />
London, England. J. Med. Vet. Mycol. 24:219-230.<br />
Morton, F.J. and G. Smith. 1963. The genera Scopulariopsis Bainier, Microascus<br />
Zukal, and Doratomyces Corda. Mycological Papers, No. 86. Commonwealth Mycological<br />
Institute, Kew, London.<br />
Nakamura, Y., R. Kano, T. Mural et. al. 2000. Susceptibility testing of Malassezia<br />
species using the urea broth microdilution method. Antimicrob. Agents. Chemother.<br />
44:2185-2186.<br />
Nishimura, K. and M. Miyaji. 1983. Studies on the phylogenesis of pathogenic “black<br />
yeasts”. Mycopathologia. 81:135-144.<br />
Nottebrock, H., H.J. Scholer and M. Wall. 1974. Taxonomy and identification of mucormycosis<br />
causing fungi. 1. Synonymity of Absidia ramosa with A. corymbifera.<br />
Sabouraudia. 12:64-74.
Descriptions of Medical Fungi 195<br />
REFERENCES<br />
Nucci, M., T. Akiti, G. Barreiros et. al. 2001. Nosocomial fungemia due to Exophiala<br />
jeanselmei var. jeanselmei and a Rhinocladiella species: newly described causes<br />
of bloodstream infection. J. Clin. Microbiol. 39:514-518.<br />
O’Donnell, K.L. 1979. Zygomycetes in culture. Palfrey Contributions in Botany 2.<br />
University of Georgia. pp 257.<br />
Onions, A.H.S., D. Allsopp and H.O.W. Eggins. 1981. Smith’s introduction to industrial<br />
mycology. Edward Arnold.<br />
Padhye, A.A., and L. Ajello 1988. Simple method of inducing sporulation by Apophysomyces<br />
elegans and Saksenaea vasiformis. J. Clin. Microbiol. 26:1861-1863.<br />
Padhye, A.A., G. Koshi, V. Anandi et. al. 1988. First case of subcutaneous zygomycosis<br />
caused by Saksenaea vasiformis in India. Diagn. Microbiol. Infect. Dis.<br />
9:69-77.<br />
Paphitou, N.I., L. Ostrosky-Zeichner, V.L. Paetznick et. al. 2002. In vitro antifungal<br />
susceptibility of Trichosporon species. Antimicrob. Agents. Chemother. 46:1144-<br />
1146.<br />
Pfaller, M.A., F. Marco, S.A. Messer and R,N. Jones. 1998. In vitro activity of two<br />
echinocandin derivatives, LY303366 and MK-0991 (L-743,792), against clinical isolates<br />
of Aspergillus, Fusarium, Rhizopus, and other filamentous fungi. Diagn. Microbiol.<br />
Infect. Dis. 30:251-255.<br />
Pfaller, M.A., S.A. Messer, R.J. Hollis et. al. 2002a. Antifungal activities of posaconazole,<br />
ravuconazole and voriconazole compared with those of itraconazole and<br />
amphotericin B against 239 clinical isolates of Aspergillus spp. and other filamentous<br />
fungi: report from SENTRY antimicrobial surveillance program, 2000. Antimicrob.<br />
Agents Chemother. 46:1032-1037.<br />
Pfaller, M.A., S.A. Messer, R.J. Hollis et. al. 2002b. In vitro activities of ravuconazole<br />
and voriconazole compared with those of four approved systemic antifungal<br />
agents against 6,970 clinical isolates of Candida spp. Antimicrob. Agents Chemother.<br />
46:1723-1727.<br />
Pfaller, M.A., D.J. Diekema, S.A. Messer et. al. 2003. In vitro activities of voriconazole,<br />
posaconazole, and four licensed systemic antifungal agents against Candida<br />
species infrequently isolated from blood. J. Clin. Microbiol. 41:78-83.<br />
Pfaller, M.A., L. Boyken, R.J. Hollis et. al. 2006. In vitro susceptibility of Candida<br />
spp. to Caspofungin: four years of global surveillance. J. Clin. Microbiol. 44:760-<br />
763.<br />
Pfaller, M.A. and D.J. Diekema. 2007. The epidemiology of invasive candidiasis: a<br />
persistent public health problem. Clin. Microbiol. Rev. 20:133-163.<br />
Pitt, J.I. 1979. The genus Penicillium and its teleomorphic states Eupenicillium and<br />
Talaromyces. Academic Press.<br />
Pore, R.S. 1985. Prototheca taxonomy. Mycopathologia. 129:129-139.<br />
Pritchard, R.C., D.B. Muir, K.H. Archer et. al. 1986, Subcutaneous zygomycosis<br />
due to Saksenaea vasiformis in an infant. Med. J. Aust. 145:630-631.<br />
Pujol, I., C. Aguilar, J. Gene, J. Guarro. 2000. In vitro antifungal susceptibility of<br />
Alternaria spp. and Ulocladium spp. J. Antimicrob. Chemother. 46:337.<br />
Punithalingam, E. 1979. Sphaeropsidales in culture from humans. Nova Hedwigia.<br />
31:119-158.<br />
Raper, K.B. and D.I. Fennell. 1965. The genus Aspergillus. William & Wilkins Co.,<br />
Baltimore.
196<br />
Descriptions of Medical Fungi<br />
REFERENCES<br />
Raper, K.B. and C.H. Thom. 1949. A manual of the penicillia. William & Wilkins Co.,<br />
Baltimore.<br />
Ramirez, C. 1982. Manual and atlas of the Penicillia. Elsevier Biomedical Press.<br />
Rebell, G., and D. Taplin. 1970. The Dermatophytes. 2nd. revised edition. University<br />
of Miami Press, Coral Gables, Florida. USA.<br />
Richter, S.R., R.P. Galask, S.A. Messer et. al. 2005. Antifungal susceptibility of Candida<br />
species causing vulvovaginitis and epidemiology of recurrent cases. J. Clin.<br />
Microbiol. 43:2155-2162.<br />
Rippon, J.W. 1988. Medical Mycology. 3rd Edition. W.B. Saunders Co.<br />
Rippon, J.W., P.M. Arnow, R.A. Larson et. al. 1985. “Golden tongue” syndrome<br />
caused by Ramichloridium schulzeri. Arch. Dermatol. 121:892-894.<br />
Rodero, L., M. Cuenca-Estrella, S. Cordoba et. al. 2002. Transient fungemia caused<br />
by an amphotericin B-resistant isolate of Candida haemulonii. J. Clin. Microbiol.<br />
40:2266-2269.<br />
Rodriguez-Tudela, J.L., T.M. Diaz-Guerra, E. Mellado et. al. (2005). Susceptibility<br />
patterns and molecular identification of Trichosporon species. Antimicrob. Agents<br />
Chemother. 49:4026-4034.<br />
Sabatelli, F., R. Patel, P.A. Mann et al. 2006. In vitro activities of posaconazole,<br />
fluconazole. itraconazole, voriconazole, and amphotericin B against a large collection<br />
of clinically important moulds and yeasts. Antimicrob. Agents Chemother.<br />
50:2009-2015.<br />
Saksena, S.B. 1953. A new genus of Mucorales. Mycologia 45:426-436<br />
Salkin, I.F., M.R. McGinnis, M.J. Dykstra and M.G. Rinaldi. 1988. Scedosporium<br />
inflatum, an emerging pathogen. J. Clin. Microbiol. 26:498-503.<br />
Samson, R.A. 1969. Revision of the genus Cunninghamella (Fungi, Mucorales).<br />
Proceedings of the Koninklijke Nederlandse Akademie van Wetenschappen, ser.<br />
C, 72:322-335.<br />
Samson, R.A. 1974. Paecilomyces and some allied hyphomycetes. Studies in Mycology<br />
No. 6. Baarn, The Netherlands.<br />
Samson, R.A., E.S. Hoekstra, J.C. Frisvad and O. Filtenborg. 1995. Introduction<br />
to food-borne fungi. Centraalbureau voor Schimmelcultures, P.O.Box 273, 3740 AG<br />
BAARN, The Netherlands.<br />
Samson, R.A. and J.I. Pitt. 1990. Modern concepts in Penicillum and Aspergillus<br />
classification. Plenum Press, New York, USA.<br />
Santos D.A., and J.S. Hamdan. 2006. In vitro antifungal oral drug and drug-combination<br />
activity against onychomycosis causative dermatophytes. Medical Mycology.<br />
44:357-362.<br />
Schell, W.A., M.R. McGinnis and D. Borelli. 1983. Rhinocladiella aquaspora a new<br />
combination for Acrotheca aquaspersa. Mycotaxon 17:341-348<br />
Schipper, M.A.A. 1976. On Mucor circinelloides, Mucor racemosus and related species.<br />
Stud Mycol. 12: 1-40.<br />
Schipper, M.A.A. 1978. 1. On certain species of Mucor with a key to all accepted species.<br />
2. On the genera Rhizomucor and Parasitella. Studies in Mycology No.17.<br />
Centraalbureau voor Schimmelcultures, Baarn, The Netherlands.<br />
Schipper, M.A.A. 1984. A revision of the genus Rhizopus 1. The Rhizopus stolonifergroup<br />
and Rhizopus oryzae. Stud. Mycol. 25: 1-19.<br />
Schipper, M.A.A. and Stalpers, J.A. 1984. A revision of the genus Rhizopus II. The<br />
Rhizopus microsporus group. Stud. Mycol. 25: 30-34.
Descriptions of Medical Fungi 197<br />
REFERENCES<br />
Schipper, M.A.A. and Stalpers, J.A. 2003. Zygomycetes: The Order Mucorales. In<br />
Howard, D.H. (ed.), Pathogenic Fungi in Humans and Animals. 2 nd edition, Marcel<br />
Dekker Inc., New York, 67-125.<br />
Schipper, M.A.A., M.M. Maslen, G.G. Hogg et. al. 1996. Human infection by Rhizopus<br />
azygosporus and the occurrence of azygospores in Zygomycetes. J. Med. Vet.<br />
Mycol. 34: 199-203.<br />
Scholer, H.J., E. Müller and M.A.A. Schipper. 1983. Mucorales. In: Howard DH,<br />
ed. Fungi pathogenic for humans and animals, Part A Biology. Marcel Dekker Inc<br />
New York, pp 9-59.<br />
Serrano, M.C., D. Morilla, A. Valverde et. al. 2003. Comparison of Etest with modified<br />
broth microdilution method for testing susceptibility of Aspergillus spp. to voriconazole.<br />
J. Clin. Microbiol. 41:5270-5272.<br />
Seth, H.K. 1970. A monograph of the genus Chaetomium. Nova Hedwigia 37:1-<br />
134.<br />
Shipton, W.A. and P. Zahari. 1987. Sporulation media for Basidiobolus species. J.<br />
Med. Vet. Mycol. 25:323-327.<br />
Sigler, L., S.P. Abbott and A.J. Woodgyer. 1994. New records of nail and skin infection<br />
due to Onychocola canadensis and description of its teleomorph Arachnomyces<br />
nodosetosus sp. nov. J. Med. Vet. Mycol. 32:275-285.<br />
Sigler, L. and H. Congly. 1990. Toenail infection caused by Onychocola canadensis<br />
gen. et. sp. nov. J. Med. Vet. Mycol. 28:405-417.<br />
Sigler, L., L.M. de la Maza, G. Tan et. al. 1995. Diagnostic difficulties caused by a<br />
nonclamped Schizophyllum commune isolate in a case of fungus ball of the lung.<br />
J. Clin. Micro. 33:1979-1983.<br />
Sigler, L. and J.W. Carmichael. 1976. Taxonomy of Malbranchea and some other<br />
hyphomycetes with arthroconidia. Mycotaxon. 4:349-488.<br />
Singh, J., D. Rimek and R. Kappe. 2005. In vitro susceptibility of 15 strains of zygomycetes<br />
to nine antifungal agents as determined by the NCCLS M38-A microdilution<br />
method. Mycoses. 48:246-250.<br />
Simmons, E.G. 1967. Typification of Alternaria, Stemphylium and Ulocladium. Mycologia.<br />
59:67-92.<br />
Sivanesan, A. 1987. Graminicolous species of Bipolaris, Curvularia, Drechslera, Exserohilum<br />
and their teleomorphs. Mycological Paper No. 158. CAB International,<br />
U.K.<br />
Staib F. (1987). Cryptococcus in AIDS Mycological Diagnostic and Epidemiological<br />
Observations. Aids Forshung (AIFO)2, 363-382.<br />
Steele, T., G.W. Kaminski and D. Hansman. 1977. A case of coccidioidomycosis in<br />
Australia. Med. J. Aust 1:968-969.<br />
Sorrell, T. C. 2001. Cryptococcus neoformans variety gattii. Med, Mycol. 39:155-<br />
168.<br />
Strinivasan, M.C. and M.J. Thirumalachar. 1965. Basidiobolus species pathogenic<br />
for man. Sabouraudia. 4:32-34.<br />
Sugar, A.M. and X.P. Liu. 1996. In vitro and in vivo activities of SCH 56592 against<br />
Blastomyces dermatitidis. Antimicrob. Agents Chemother. 40:1314-1316.<br />
Sun, Q.N., A.W. Fothergill, D.I. McCarthy et. al. 2002. In vivo activities of posaconazole,<br />
itraconazole, voriconazole, amphotericin B, and fluconazole against 37 clinical<br />
isolates of zygomycetes. Antimicrob. Agents Chemother. 46: 1581-1582.
198<br />
Descriptions of Medical Fungi<br />
REFERENCES<br />
Sutton, B.C. 1980. The Coelomycetes, fungi imperfecti with pycnidia, acervuli and<br />
stromata. Commonwealth Mycology Institute, Kew, London.<br />
Sutton, B.C. and B.J. Dyko. 1989. Revision of Hendersonula. Mycol. Res. 93:466-<br />
488.<br />
Tintelnot, K. and B. Nitsche. 1989. Rhizopus oligosporus as a cause of mucormycosis<br />
in man. Mycoses. 32: 115-118.<br />
Trilles, L., B. Fernandez-Torres, M. dos Santos Lazera et. al. 2004. In vitro antifungal<br />
susceptibility of Cryptococcus gattii. J. Clin. Microbiol 42:4815-4817.<br />
Vanbreusegham, R, CH. de Vroey and M. Takashio. 1978. Practical guide to medical<br />
and veterinary mycology. Mason Publishing USA, Inc.<br />
Van Oorschot, C.A.N. 1980. A revision of Chrysosporium and allied genera. Studies<br />
in Mycology No.20. Centraalbureau voor Schimmelcultures, Baarn, The Netherlands.<br />
Velegraki, A., E.C. Alexopoulos, S. Kritikou et. al. 2004. Use of fatty acid RPMI<br />
1640 media for testing susceptibilities of eight Malassezia species to the new triazole<br />
posaconazole and six established antifungal agents by a modified NCCLS<br />
M27-A2 microdilution method and Etest. J. Clin. Microbiol. 42:3589-3593.<br />
Vitale, R.G. and G.S. de Hoog. 2002. Molecular diversity, new species and antifungal<br />
susceptibilities in the Exophiala spinifera clade. Medical Mycology. 40:545-556.<br />
Voigt, K., E. Cigelnik and K. O’Donnell, K. 1999. Phylogeny and PCR identification<br />
of clinically important zygomycetes based on nuclear ribosomal-DNA sequence<br />
data. J. Clin. Microbiol. 37: 3957-3964.<br />
Weitzman, I. 1984. The case for Cunninghamella elegans, C. bertholletiae and C.<br />
echinulata as separate species. Trans. Br. Mycol. Soc. 83:527-528.<br />
Weitzman, I., M.R. McGinnis, A.A. Padhye and L. Ajello. 1986. The genus Arthroderma<br />
and its later synonym Nannizzia. Mycotaxon. 25:505-505.<br />
Weitzman, I. and M.Y. Crist. 1980. Studies with clinical isolates of Cunninghamella.<br />
II. Physiological and morphological studies. Mycologia. 72: 661-669.<br />
Wieden, M.A., Steinbronn, K.K., Padhye, A.A. et. al. 1985. Zygomycosis caused by<br />
Apophysomyces elegans. J Clin Microbiol. 22: 522-526.<br />
Wilson, C.M., E.J. O’Rourke, M.R. McGinnis et. al. 1990. Scedosporium inflatum:<br />
Clinical spectrum of a newly recognised pathogen. J. Infect. Dis. 161:102-107.<br />
Woodward, A., C. McTigue, G. Hogg et. al. 1992. Mucormycosis of the neonatal<br />
gut: a new disease or a variant of necrotizing entercolitis? J. Pediatr. Surg. 27:<br />
737-740.<br />
Yarrow, D. and S.A. Meyer. 1978. Proposal for the amendment of the diagnosis of<br />
the genus Candida Berkhout nom. cons. Int. J. Syst. Bacteriol. 28:611-615.<br />
Yuan, G.F. and S.C. Jong. 1984. A new obligate azygosporic species of Rhizopus.<br />
Mycotaxon. 20: 397-400.<br />
Zycha, H., R. Siepmann and G. Linnemann. 1969. Mucorales, eine Beschreibung<br />
aller Gattungen und Arten dieser Pilzgruppe. Cramer Lehre, 355p.


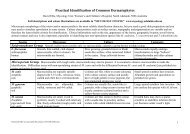




![List for QAP Fungi [2006].](https://img.yumpu.com/36263775/1/184x260/list-for-qap-fungi-2006.jpg?quality=85)


